Breakthrough: HPV Vaccine Reduces Vaginal Cancer Risk
This article examines the significant breakthrough in reducing the risk of vaginal cancer through Human Papillomavirus (HPV) vaccinations. It provides an in-depth exploration of HPV, its link to vaginal cancer, the impact of the HPV vaccine, and the future prospects for prevention. Real-life accounts and ongoing research efforts are also spotlighted. Navigating access and costs associated with the vaccine are discussed, assisting readers in making informed health decisions.

Key Takeaways
- HPV vaccination at a young age significantly reduces the risk of future vaginal cancer.
- HPV vaccines have reduced the incidence of cervical, vaginal, and other HPV-related cancers.
- The vaccine stimulates the body's immune system to recognize and fight the human papillomavirus.
- Studies show a significant reduction in the risk of developing vaginal cancer with the HPV vaccine.
Understanding the Human Papillomavirus (HPV)
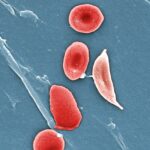
To comprehend the significant reduction in vaginal cancer risk, it is essential to understand the role of the Human Papillomavirus (HPV), which is responsible for two-thirds of vaginal cancer cases. HPV transmission occurs through intimate skin-to-skin contact, often during sexual activity. It is not solely an issue of sexual promiscuity; even individuals who have had only one partner can contract the virus. The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for boys and girls at age 11 or 12, but it can be given as early as 9 years old. Vaccination at a young age is crucial because it should occur before potential exposure to HPV, significantly reducing the risk of future vaginal cancer. Understanding HPV transmission and following HPV vaccination guidelines are key to cancer prevention.
The Link Between HPV and Vaginal Cancer
Understanding the link between HPV and vaginal cancer involves studying the virus's role in cellular changes, and recognizing the significant risk it poses for the development of this type of cancer. HPV or Human Papillomavirus is a group of viruses that includes more than 100 different strains or types, some of which are linked to cancer. Understanding HPV transmission is crucial as it is mainly transmitted through sexual contact. The risk of developing vaginal cancer increases with persistent HPV infection. Fortunately, HPV vaccination guidelines recommend vaccination for both boys and girls at ages 11 or 12, but can be given as early as age 9. This timely vaccination can significantly reduce the risk of HPV-related cancers, including vaginal cancer.
The Emergence of HPV Vaccines
Often touted as a medical marvel, the HPV vaccine emerged in the early 21st century, and has since been extensively studied for its effectiveness in preventing HPV-related cancers. The development was a major milestone in understanding HPV transmission, fundamentally changing the approach towards the viral infection. The vaccine primarily targets the high-risk HPV types that often lead to cervical, vaginal, and other HPV-related cancers. The impact of HPV on reproductive health is substantial, with the virus causing almost all cases of cervical cancer and a significant proportion of vaginal and vulvar cancers. The emergence of the HPV vaccines has, therefore, provided an essential tool in reducing the incidence of these cancers and improving reproductive health worldwide.
How HPV Vaccines Work
The HPV vaccine's mechanism of action involves stimulating the body's immune system to recognize and fight the human papillomavirus, and it has been proven to be highly effective in preventing infection. The vaccine introduces a harmless protein that resembles the virus, which the immune system then learns to attack. When later confronted with the actual HPV virus, the immune system can respond more quickly and robustly. In terms of HPV vaccine effectiveness, it has been shown to significantly reduce the incidence of HPV-related cancers and genital warts. Concerning HPV vaccine safety, it has undergone rigorous testing and monitoring, confirming its overall safety. Side effects, if any, are typically mild and transient, further affirming the vaccine's crucial role in cancer prevention.
Studying the Impact of HPV Vaccine on Vaginal Cancer Risk
Researchers' exploration into the impact of the HPV vaccine reveals a significant reduction in the risk of developing vaginal cancer. Studies have been conducted to understand the HPV vaccine effectiveness, particularly in the long term. Preliminary results indicate a substantial decrease in the likelihood of HPV-related infections, which are responsible for the majority of vaginal cancer cases. The long term impact of this vaccine is encouraging; it not only minimizes immediate risks, but also ensures sustained protection. Continued study is necessary to further validate these findings and to understand any potential side effects. Nonetheless, the role of the HPV vaccine in mitigating vaginal cancer risk underscores its importance in women's health.
Key Findings: HPV Vaccine and Vaginal Cancer
Significant reductions in vaginal cancer incidence and the promising long-term effectiveness of the HPV vaccine constitute the key findings of recent studies, offering hope and a new line of defense for women worldwide. These findings emerge from the rigorous process of studying vaccine effectiveness, taking into account numerous variables and large data sets. The long term vaccine impact, as revealed by these studies, has shown a consistently high degree of protection against HPV, the virus responsible for a majority of vaginal cancer cases. This breakthrough underlines the critical role of HPV vaccination in mitigating vaginal cancer risk, reinforcing its position as a key preventive measure. These results underscore the importance of continued research, in order to substantiate these promising findings and to explore further improvements in HPV vaccine effectiveness.
Implications of the HPV Vaccine Breakthrough
Undoubtedly, this breakthrough in HPV vaccination not only sets a new precedent in cancer prevention strategies, but also prompts a reevaluation of current public health policies towards widespread vaccination. Understanding vaccine effectiveness is critical in this context. The HPV vaccine's ability to significantly reduce the risk of vaginal cancer underscores its potency and highlights the necessity for its broader implementation. Moreover, examining the long-term effects of HPV vaccination is crucial to ensure its safety and efficiency. These effects, promisingly, have been largely positive, further endorsing the vaccine's potential. Consequently, this breakthrough paves the way for a paradigm shift in our approach to cancer prevention, underscoring the importance of vaccines in public health strategy.
The Importance of Early HPV Vaccination
In the fight against vaginal cancer, getting the HPV vaccine at an early age is crucial, and it serves as an effective method to significantly lower the risk of this disease. The early vaccination benefits are multifold; they extend beyond immediate protection to long-term health preservation. Studies show that the vaccine effectiveness is maximized when administered before exposure to HPV, typically before sexual debut. This preemptive protection inhibits the virus's ability to establish a persistent infection, which is a significant precursor to the development of vaginal cancer. Therefore, early HPV vaccination is not just a recommended health strategy, it is a vital preventive measure against a potential life-threatening disease, underscoring the necessity of timely immunization in the healthcare agenda.
Handling HPV Vaccine Side Effects
While the benefits of the HPV vaccine in reducing the risk of vaginal cancer are clear, addressing potential side effects is also a key component in managing its overall impact on patients' health. Understanding vaccine side effects, which may include mild fever, headache, or pain at the injection site, is crucial for patient comfort and confidence. It's important to note that these side effects are generally short-lived and far outweighed by the preventative effects of the vaccine. Managing vaccine side effects can involve simple steps like taking over-the-counter pain medication or applying a cool compress to the injection site. Dialogue between healthcare providers and patients is vital in addressing concerns, easing fears, and ensuring the best possible health outcomes.
Navigating HPV Vaccine Access and Costs
As you consider the HPV vaccine, understanding how to navigate access to the vaccine and manage its associated costs is an essential step in the process. HPV vaccine access can vary by location, insurance coverage, and individual healthcare providers. Many health insurance plans cover the cost of the vaccine as part of preventative care, and the Vaccines for Children (VFC) program provides vaccines at no cost to children who might not otherwise be vaccinated because of inability to pay. Directly contact your healthcare provider or local health department to discuss HPV vaccine access. Vaccine costs can be a deterrent for some, but it's crucial to weigh these against the potential health and financial implications of HPV-related diseases, including vaginal cancer.
The Future of HPV Vaccines and Vaginal Cancer Prevention
The scientific community's progress in HPV vaccine development and its implementation is promising for the future of vaginal cancer prevention, but there remain significant challenges that require ongoing research and strategic approaches. Future research must focus on improving the vaccine's efficacy, accessibility, and acceptance, particularly in underprivileged regions. The global impact of HPV vaccines can be greatly enhanced if these focuses are addressed effectively. Studies should also explore new HPV strains, their effects, and potential countermeasures. A concerted global effort is needed to ensure these vaccines reach all corners of the world, reducing the burden of vaginal cancer. In the face of these challenges, the promise of HPV vaccines for preventing vaginal cancer remains a beacon of hope.
Real Stories: Women, HPV Vaccination, and Vaginal Cancer Survival
Although statistics and clinical data provide a comprehensive view of the HPV vaccine's impact on vaginal cancer, it is through the personal narratives of women who have undergone HPV vaccination and successfully battled vaginal cancer that the true picture of this medical breakthrough emerges. Survivor testimonials have been instrumental in painting a vivid image of vaccine effectiveness. Martha, a 35-year-old survivor, credits the HPV vaccine for her cancer-free status today. Similarly, 40-year-old Susan, another survivor, referred to the vaccine as a "lifesaver." These stories highlight the transformative power of the HPV vaccine in combating vaginal cancer. They serve as a beacon of hope, emphasizing the vaccine's role as a crucial tool in the ongoing fight against this form of cancer.
Continual Research: The Ongoing Fight Against Vaginal Cancer
Over two hundred ongoing research studies worldwide are currently dedicated to advancing our understanding of vaginal cancer and enhancing the effectiveness of preventative measures such as the HPV vaccine. This relentless pursuit of knowledge underscores the vital importance of continual investigation into this disease. The primary focus of this ongoing research is to discover novel methods for early detection, refine therapeutic approaches, and verify vaccine effectiveness. Such diligent investigations have already reaped rewards, the most notable being the HPV vaccine which has significantly reduced the risk of vaginal cancer. Yet, the fight continues. As each new piece of information is gleaned, the medical community moves one step closer to the ultimate goal: eradicating vaginal cancer altogether.
Frequently Asked Questions
How Does the Treatment for Vaginal Cancer Differ if It Is Hpv-Related or Not?
The treatment for vaginal cancer does not typically differ based on whether it is HPV-related or not. However, identifying specific HPV strains could be beneficial in determining the potential risk of cancer progression. Regular monitoring and follow-up exams are crucial in managing cancer, especially for HPV-associated cases. Treatments may involve surgery, radiation therapy, chemotherapy, or a combination, depending on the stage and type of the cancer.
Are There Any Lifestyle Changes That Can Help Prevent Vaginal Cancer?
Certain lifestyle modifications can aid in the prevention of vaginal cancer. Maintaining a balanced diet with nutrient-rich foods can potentially reduce the risk. Dietary impacts are significant as they contribute to overall health. Regular exercise also benefits the body by boosting the immune system and maintaining healthy body weight, which is crucial for cancer prevention. Additionally, avoiding HPV infection through vaccination and safe sexual practices can also help. It's essential to consult healthcare professionals for personalized advice.
Can Men Also Get Hpv-Related Cancers and Would the Vaccine Work for Them Too?
Yes, men are also susceptible to HPV-related cancers such as penile, anal, and oropharyngeal cancers. Men's vaccination with the HPV vaccine has been shown to be effective in reducing these risks. HPV transmission is not gender-specific; both sexes can contract and transmit the virus. Hence, HPV vaccination is a crucial preventative measure for both men and women.
Are There Any Other Vaccines in Development for Preventing Hpv-Related Cancers?
Indeed, there are ongoing research studies aimed at developing more effective vaccines to prevent HPV-related cancers. Emphasis is placed on enhancing vaccine efficacy through targeting multiple HPV strains and improving immune responses. Future research is expected to reveal novel vaccination strategies, potentially offering broader protection against the plethora of HPV-related malignancies. However, the timeline and success of these developments are yet to be determined.
How Does the HPV Vaccine Interact With Other Ongoing Treatments or Medications?
The interaction of the HPV vaccine with other treatments or medications, often termed as 'Vaccine Interactions' and 'Medication Compatibility', is generally minimal. The vaccine is usually well-tolerated and does not interfere with the effectiveness of other medications. However, it is always recommended to inform your healthcare provider about any ongoing treatments or medications to ensure a safe and effective vaccination process. Each individual's health condition and medication regimen may require personalized advice.
Conclusion
In summary, HPV vaccinations present a promising solution to reducing the risk of vaginal cancer. Despite numerous challenges such as accessibility and cost, their potential impact is significant. The shared experiences of women who survived vaginal cancer after HPV vaccination underscore this fact. Continual research is crucial in the fight against vaginal cancer, with the ultimate goal being the development of specific preventive measures and screening guidelines. Connecting with the National Cancer Institute provides further information and support.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.