Goiter Development and AFFF: Assessing Other Risk Factors
We've found that alongside traditional factors like iodine deficiency, exposure to Aqueous Film Forming Foam (AFFF) substantially raises the risk of goiter development. AFFF, used extensively in firefighting, contains PFAS chemicals which disrupt thyroid functions, leading to potential thyroid enlargement. Our analysis highlights the importance of monitoring thyroid health, particularly in individuals with occupational AFFF exposure such as firefighters and military personnel. Additionally, we emphasize the role of genetics, environmental pollution, and lifestyle choices in goiter susceptibility. Understanding these diverse risk factors is essential for effective prevention and management strategies. Our continued examination reveals further insights into mitigating these risks.
Key Takeaways
- AFFF exposure is linked to thyroid dysfunction due to PFAS, increasing goiter risk.
- Iodine deficiency remains a major risk factor for goiter development worldwide.
- Genetic predispositions can significantly influence individual susceptibility to goiter.
- Environmental pollutants like PCBs and dioxins can disrupt thyroid function, raising goiter risk.
- Lifestyle factors, including diet, tobacco, and alcohol use, affect thyroid health and goiter likelihood.
Understanding Goiter

Exploring the multifaceted nature of goiter, we discover it's essentially an enlargement of the thyroid gland, appearing in various forms such as diffuse, nodular, or multinodular. This condition, a visible sign of underlying thyroid diseases, demands our attention not only due to its physical manifestation but also because it signals the importance of adequate iodine intake for thyroid health. While iodine deficiency is a significant global cause, we're steering clear of delving into this aspect for now, focusing instead on other factors that contribute to the development of goiter.
Understanding goiter's complexity, it's crucial to recognize that genetics, demographics, and environmental influences also play a pivotal role. These factors can predispose individuals to thyroid diseases, with goiter being a common outcome. Notably, the prevalence of goiter shows a distinct gender disparity, with females being more susceptible than males. This observation underscores the necessity for gender-specific research and intervention strategies in managing thyroid health. Additionally, while racial differences in goiter prevalence are not as pronounced, this does not diminish the importance of considering demographic variables in understanding and addressing thyroid diseases.
Iodine Deficiency Impact
We'll explore how iodine deficiency, an important environmental factor, greatly influences the worldwide prevalence of goiter. This condition, marked by the enlargement of the thyroid gland, demonstrates the essential role iodine plays in our health. Insufficient iodine intake doesn't just risk the development of various types of goiter; it fundamentally disrupts the synthesis of thyroid hormones, essential for our metabolic processes.
Populations with low iodine status find themselves at a notably higher risk. The connection between iodine deficiency and the thyroid gland is clear: without sufficient iodine, the gland struggles to produce necessary hormones, leading to its enlargement as it attempts to compensate. This condition affects diverse demographic groups, underscoring the universal need for sufficient iodine intake to maintain thyroid health.
Addressing this deficiency is possible and critical. Dietary changes or supplementation programs offer viable solutions to prevent the onset of goiter in those most at risk. By understanding the impact of iodine deficiency, we're better positioned to combat its prevalence. It's not merely about managing a health condition but ensuring the well-being of communities globally.
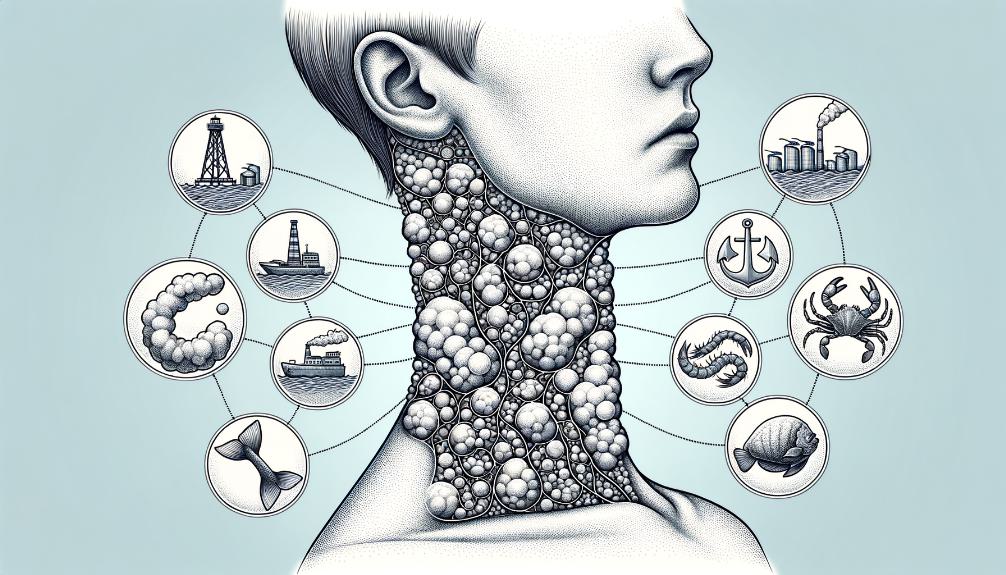
AFFF Exposure Risks

Shifting our focus to AFFF exposure, it's crucial to understand how this can significantly increase the risk of thyroid dysfunction and goiter. The presence of per- and polyfluoroalkyl substances (PFAS) in Aqueous Film Forming Foam (AFFF) poses a notable threat to the regulation of thyroid hormones. These chemicals are well-known for their ability to disrupt endocrine functions, and their connection with thyroid issues is particularly concerning.
Studies have shown that exposure to PFAS can result in thyroid enlargement and the development of nodules that closely resemble goiter. This link highlights the importance of being mindful of the environments and professions that may lead to higher exposure levels to these harmful substances. Specifically, firefighters, military personnel, and airport workers are identified as groups at an increased risk due to their frequent and potentially intense contact with AFFF.
Given these dangers, it becomes crucial for individuals with a history of AFFF exposure to undergo regular monitoring of their thyroid function. This proactive approach is essential in evaluating the risk factors for goiter development among those exposed to AFFF. By understanding the chemical dynamics at play and the populations most at risk, we can better navigate the prevention and management of thyroid dysfunction and goiter.
It's evident that the consequences of AFFF exposure go beyond immediate health risks, highlighting the need for thorough health surveillance among affected individuals. The association between PFAS and thyroid health is a critical aspect in understanding the complete extent of AFFF's impact on human health.
Genetic Factors
Genetic factors significantly influence an individual's risk of developing goiter, emphasizing the importance of understanding our genetic makeup in managing thyroid health. Studies have shown that mutations in various genes play a pivotal role in goiter development, highlighting the genetic complexity of this condition. These genetic variations not only make individuals more susceptible to thyroid gland enlargement but also increase the risk of autoimmune diseases or thyroid cancer, which are significant contributors to goiter.
Moreover, a family history of thyroid disorders is a critical genetic factor in determining an individual's predisposition to developing goiter. It's evident that if there's a pattern of thyroid-related issues within a family, the odds of encountering similar problems are significantly higher. This correlation underscores the need for those with a family history of thyroid disorders to be more vigilant about their thyroid health.
Understanding the genetic basis of goiter is not just about identifying risk; it's about enabling personalized risk assessment and management strategies for those affected. By recognizing the specific genetic factors at play in each case, healthcare providers can tailor their approach to prevention and treatment, potentially mitigating the impact of the condition.
In essence, the intricate relationship between genetic factors and the development of goiter cannot be overstated. As we explore deeper into the genetics of thyroid disorders, we're not only uncovering the causes behind these conditions but also paving the way for more effective, personalized interventions. Acknowledging and investigating these genetic influences is essential for anyone looking to manage or understand their thyroid health better.
Environmental Influences

We've observed that environmental factors play a significant role in the development of goiter, particularly through industrial pollution exposure and dietary iodine deficiency. These elements, ranging from the quality of air and water in industrial areas to the iodine content in daily diets, directly impact the prevalence of this condition. It's critical we examine how these environmental influences contribute to goiter, ensuring a thorough understanding of its risk factors.
Industrial Pollution Exposure
Industrial pollution exposure, including heavy metals and toxic chemicals, has been linked to a higher risk of goiter development. We've observed that pollutants such as polychlorinated biphenyls (PCBs) and dioxins can greatly disturb thyroid function, contributing to the formation of goiter. Research indicates that people residing near industrial zones with elevated pollution levels have an increased likelihood of encountering thyroid disorders, including goiter. The inflammation of the thyroid gland, potentially triggered by these industrial pollutants, often leads to the gland's enlargement, a hallmark of goiter. It's essential we push for reduced industrial pollution and limit exposure to these harmful substances, aiming to prevent not only goiter but other thyroid-related conditions as well.
Dietary Iodine Deficiency
While industrial pollution exposure heavily influences goiter development, another key environmental factor worth examining is dietary iodine deficiency. We've learned that insufficient iodine intake disrupts thyroid hormone synthesis, leading to an enlarged thyroid gland. This condition, known primarily as goiter, highlights the critical role iodine plays in the production of thyroid hormones T3 and T4, which are essential for regulating metabolism. Globally, regions with low iodine levels in the soil witness higher rates of goiter due to iodine deficiency. It's clear that ensuring adequate daily iodine intake is fundamental in preventing iodine deficiency-related goiter. We must prioritize understanding and addressing these environmental influences to mitigate the risk of goiter development effectively.
Gender Disparities
We're now turning our attention to gender disparities in goiter development, a critical aspect that deserves our focus. It's evident that hormonal influence has a substantial impact on women, while men's risk factors are being analyzed to understand their susceptibility. Additionally, we're committed to addressing gender-based research gaps to guarantee a thorough understanding and effective prevention strategies.
Hormonal Influence on Women
Given the substantial role hormones play, it's imperative to understand how estrogen fluctuations during key life stages such as puberty, pregnancy, and menopause can heighten women's risk of developing goiter. Estrogen levels play a vital role in thyroid hormone regulation, which is important in the context of goiter formation. This hormonal interplay makes thyroid disorders, particularly goiter, more common among women. Acknowledging that these estrogen-induced changes in thyroid function emphasize the need for diligent monitoring of thyroid health in women. Their increased susceptibility to goiter, driven by these hormonal dynamics, requires a more nuanced approach to understanding and managing thyroid health. Addressing this gender disparity effectively can have a significant impact on the prevention and treatment of goiter in women.
Mens Risk Factors Analyzed
Despite the higher prevalence of goiter in women, it's important to explore the risk factors that can lead to its development in men and understand the gender-based disparities. It's recognized that gender disparities in goiter incidence hint at hormonal or genetic factors potentially playing a significant role in the increased risk for women. However, this doesn't mean men are immune. Differences in thyroid hormone levels between genders suggest that while the impact might be less pronounced in men, it's still a significant area of concern. Understanding these gender disparities is vital in tailoring treatment and prevention strategies effectively for men, ensuring that their risk factors are not overlooked simply because they are less likely to develop goiter compared to women.
Gender-Based Research Gaps
Understanding the gender disparities in goiter development necessitates closing significant research gaps, particularly in how hormonal, autoimmune, and genetic factors distinctly affect women. We've found that women are more prone to goiter, with estrogen levels, among other factors, playing an essential role. This disparity is not just a number; it's a call to action for more gender-focused research. Hormonal fluctuations during pivotal moments like puberty, pregnancy, and menopause contribute substantially. Yet, we're only scratching the surface. The specific mechanisms through which estrogen levels and autoimmune responses contribute to this gender disparity in goiter development remain underexplored. It's clear: to address these disparities effectively, we must delve deeper into understanding how these gender-specific factors influence goiter's pathophysiology and management in women.
Dietary Contributions
Our diets play a pivotal role in the health of our thyroid gland, directly influencing the risk of developing goiter through the intake of iodine and certain goitrogenic foods. It's well-documented that the thyroid gland requires iodine to produce thyroid hormones. As such, iodine deficiency is a primary risk factor for goiter. On the other hand, consuming excessive amounts of foods known as goitrogens, including cruciferous vegetables and soy products, can interfere with thyroid function and contribute to the development of goiter.
A balanced diet, rich in iodine-containing foods such as seafood, dairy products, and iodized salt, is essential for preventing iodine deficiency-related goiter. This highlights the importance of a well-rounded diet in maintaining thyroid health. However, it's also worth noting that, in regions where iodine sufficiency is achieved, excessive intake of iodine, whether through supplements or foods rich in iodine, can also lead to the formation of goiter. Consequently, moderation is key.
Understanding these dietary factors is vital for anyone looking to maintain optimal thyroid health and prevent goiter. It's not just about avoiding iodine deficiency but also about ensuring that one doesn't consume excessive amounts of iodine or goitrogenic foods that could disrupt thyroid function. As we continue to explore goiter development and its risk factors, it becomes clear that our dietary choices play a significant role in the overall health of our thyroid gland, underscoring the need for dietary awareness and balance.
Lifestyle and Goiter

We've observed how diet plays a vital role in goiter development, but our lifestyle choices extend beyond what we eat. Factors such as tobacco and alcohol use, along with the level of physical activity, greatly impact our thyroid health. It's essential that we grasp these dynamics to better manage and mitigate the risks associated with goiter.
Diets Role
Diet plays a pivotal role in the development and prevention of goiter, highlighting the importance of certain nutrients in our daily intake. We've learned that deficiencies in iodine, selenium, or vitamin A can have a substantial impact on goiter. Our diets, if not carefully managed, can increase our risk, especially when they're high in goitrogenic foods like soy, cassava, and cruciferous vegetables. Conversely, we've also seen how diets rich in iodine—think seafood and iodized salt—can be incredibly protective against goiter in those at risk of iodine deficiency. The Mediterranean diet, with its focus on fruits, vegetables, and seafood, offers a promising approach. It's clear that maintaining a balanced diet, emphasizing key nutrients like iodine and selenium, is essential for mitigating the risk of goiter development.
Tobacco and Alcohol Effects
Exploring the impact of lifestyle choices, particularly tobacco and alcohol use, reveals important risks for the development of goiter due to their harmful effects on thyroid function. Tobacco use has been linked to an increased goiter risk, as smoking can hinder the body's iodine absorption, essential for thyroid hormone production. This disruption contributes greatly to goiter prevalence among smokers. Similarly, excessive alcohol consumption poses a threat to thyroid health by disturbing hormone regulation and liver metabolism of thyroid hormones, potentially worsening goiter conditions. Both habits foster inflammation and oxidative stress, further impairing thyroid function and increasing goiter development risks. Understanding these risks is crucial in managing and preventing goiter, emphasizing the importance of addressing tobacco and alcohol use in thyroid health discussions.
Physical Activity Impact
How does engaging in regular physical activity influence the risk of developing goiter in individuals? We've discovered that regular exercise plays a vital role in mitigating the risk associated with goiter. By engaging in physical activity, individuals can help regulate their thyroid function and hormone production, which are pivotal in preventing the formation of goiter. A sedentary lifestyle, on the other hand, may lead to metabolic imbalances, adversely affecting thyroid health and fostering goiter development. Consequently, incorporating exercise into our daily routines not only promotes overall health but also directly benefits thyroid function, potentially lowering the risk of goiter occurrence. It's clear that maintaining an active lifestyle is instrumental in supporting a healthy thyroid gland and reducing the chances of goiter development.
Regional Prevalence

Understanding the regional prevalence of goiter reveals that factors such as iodine deficiency vary considerably across different parts of the world, impacting communities in distinct ways. It's important to recognize that areas like certain parts of Africa and Asia face a notably higher risk, primarily due to iodine deficiency. This condition doesn't occur in isolation; it's often exacerbated by a combination of environmental factors, including low soil iodine content, especially in mountainous regions. These geographical nuances underline the complexity of addressing goiter at a global scale.
We've observed that regional dietary habits and access to iodine-rich foods are pivotal in shaping the prevalence of goiter. Populations with limited access to seafood or iodized salt, for instance, are at an elevated risk. Additionally, environmental factors, such as pollution and industrial waste, present additional challenges by adversely affecting thyroid function. These insights underscore the intricate interplay between diet, environment, and health.
Thankfully, public health initiatives focusing on iodine supplementation and education have made strides in reducing goiter prevalence in some regions. These efforts highlight the importance of a targeted approach, tailored to address the specific needs and challenges of each area. It's a reflection of the fact that, with the right strategies, we can mitigate the impact of both iodine deficiency and environmental factors on goiter development.
As we explore further into the factors influencing goiter prevalence, it's evident that a thorough understanding and approach are vital. These efforts not only enhance our grasp of the condition but also pave the way for more effective prevention and intervention strategies.
Diagnostic Approaches
We'll explore the different diagnostic approaches for goiter, emphasizing techniques like inspection, palpation, and advanced imaging to accurately evaluate the condition. These methods are essential for understanding the extent of the thyroid enlargement and identifying any potential complications or underlying conditions.
Inspection and palpation of the thyroid gland are often the initial steps. Through palpation, clinicians can assess the gland's size, texture, and the presence of any thyroid nodules or abnormalities. This physical examination is a fundamental aspect of diagnosing goiter, allowing for a preliminary assessment before moving on to more sophisticated diagnostic tools.
The use of ultrasound stands out as a valuable tool in the diagnostic arsenal. It provides detailed images of the thyroid gland, enabling doctors to assess the size, structure, and presence of thyroid nodules with precision. Ultrasound is particularly useful for identifying and evaluating the characteristics of nodules, which may indicate a need for further investigation.
In cases where nodular goiters are detected, a fine needle aspiration biopsy may be necessary. This procedure is instrumental in evaluating the nodules for any signs of malignancy or other concerning features. It's a critical step in ensuring that any potential risks are identified and addressed promptly.
Lastly, Pemberton's sign is a clinical maneuver used to assess for substernal extension of the thyroid gland. This can help in identifying cases where the goiter extends beyond the neck, which may require specific management strategies.
Management Strategies
After diagnosing goiter, it's essential to explore various management strategies to effectively address the condition. Understanding the risk factors associated with goiter development, including hormonal imbalances, is pivotal in tailoring treatment plans that not only alleviate symptoms but also aim at stabilizing hormone production. We've identified that for stable, asymptomatic cases, watchful waiting combined with regular monitoring presents a pragmatic approach. This strategy involves vigilance over the goiter's progression without immediate medical intervention, ensuring that any changes in size or symptomatology are promptly addressed.
In scenarios where the goiter causes compression symptoms or there's a suspicion of malignancy, surgical intervention is often the recommended course of action. This decisive measure aims to remove the obstruction or potentially cancerous tissue, thereby mitigating the risk of complications. For individuals diagnosed with toxic goiters, where the thyroid gland produces an excess amount of hormones, radioiodine therapy and antithyroid drugs are viable treatment options. These methods focus on reducing hormone production to normal levels, effectively managing the condition.
Moreover, regular follow-up appointments, which include neck palpation and ultrasound imaging, are indispensable. These check-ups allow healthcare providers to closely monitor the goiter's response to the chosen management strategy and adjust the treatment plan as necessary. By considering these tailored strategies, we can make sure that individuals with goiter receive the most appropriate care, minimizing the impact of the condition on their daily lives while addressing the underlying risk factors associated with hormone production.
Preventive Measures
To effectively prevent goiter, prioritizing sufficient daily iodine intake is essential. It is clear to us that an adequate supply of iodine is vital for thyroid health, and therefore, incorporating foods rich in this mineral into our diets is a key preventive measure. Seafood, dairy products, and iodine-fortified foods play a crucial role in maintaining the necessary iodine levels to keep our thyroid functioning properly.
Moreover, we must be cautious about goitrogenic substances found in certain vegetables and soy products. These substances can interfere with iodine uptake by the thyroid, potentially leading to goiter development. It's important for us to moderate our consumption of such foods, especially in areas where iodine deficiency is prevalent.
Regular monitoring of thyroid function and size is another proactive step we can take. Early detection of any thyroid abnormalities allows for timely interventions, which can effectively prevent the progression to goiter. We advocate for regular check-ups, particularly for individuals living in iodine-deficient regions.
Educational efforts play a critical role in prevention, too. We're committed to raising awareness about the importance of iodized salt, especially in iodine-deficient areas. By educating populations about the benefits of iodized salt and encouraging a balanced diet rich in iodine-containing foods, we can significantly reduce the incidence of goiter.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.