Hip Replacement Complications
Navigating the journey to better health through hip replacement surgery can be akin to walking a tightrope, balancing benefits against potential complications. This article illuminates the hidden pitfalls, from joint loosening and blood clots to metallosis and periprosthetic fractures. Understanding these risks is paramount in making informed decisions. Join us as we delve into the complexities of hip replacement complications, providing a comprehensive guide for patients and their families in pursuit of improved quality of life.

Key Takeaways
- Hip replacement complications can include joint loosening, blood clots, change in leg length, dislocation, and fractures.
- Metal-on-metal hips can lead to complications such as metallosis (metal poisoning), tissue damage, serious conditions, and potential involvement in lawsuits.
- Drugwatch.com has been assisting patients since 2008, providing helpful and reliable information about medications and their effects.
- Risk factors for hip replacement complications include age, overall health, diabetes, smoking, substance abuse, certain medications, and a combination of risk factors. Complications can have life-altering effects for patients.
Understanding Hip Replacement Complications
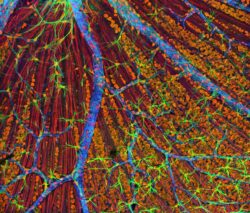
The understanding of hip replacement complications is essential for patients and caretakers alike, as it provides an in-depth knowledge of the potential risks and challenges that could arise after the surgical procedure. One such complication is Metallosis, a rare condition caused by the buildup of metallic debris in the body, often linked to metal-on-metal hip implants. This accumulation can lead to implant loosening and tissue damage, significantly impacting the patient's recovery and long-term health. Another critical factor is osteolysis, the destructive process where debris from the artificial hip accumulates in surrounding tissue, causing inflammation and eventual loosening of the implant. Understanding these complications underscores the importance of careful monitoring and post-surgical care to mitigate these risks.
The Risk of Joint Loosening Post-Surgery
How often does joint loosening occur post-surgery, and what factors might contribute to this disconcerting complication? While the frequency varies, research indicates that certain factors like age and comorbid conditions can increase the risk. The impact of age on joint loosening is significant; as the body ages, bones naturally become less dense and more susceptible to loosening. Furthermore, the role of diabetes in joint loosening is substantial, as this chronic condition can impede proper healing and increase the risk of infection, thereby contributing to joint instability. Ultimately, while advancements in surgical techniques have reduced the incidence of this complication, it remains a concern, underscoring the importance of comprehensive pre-operative assessment and careful post-operative care.
Blood Clots: A Possible Aftermath of Hip Replacement
Patients' risk of developing blood clots is a grave concern following hip replacement surgery. These clots can form due to a decrease in mobility during recovery, posing a potentially life-threatening risk if they travel to the lungs. Long term effects of metal debris, such as Metallosis and Osteolysis, can exacerbate this issue by causing inflammation and reducing the body's ability to dissolve clots. Preventing Periprosthetic Fractures is another key strategy to reduce blood clot risk. Fractures can lead to immobility, further increasing the chance of clot formation. Therefore, it's critical for healthcare providers to monitor patients closely post-surgery, ensuring early detection and treatment of any complications, such as blood clots, to optimize patient outcomes.
How Hip Replacement Can Lead to Change in Leg Length
Undergoing hip replacement surgery often results in a change in leg length, and this alteration can lead to a range of complications. This is a significant issue leading to a number of hip replacement lawsuits. The change can affect a patient's balance, gait, and overall mobility, potentially leading to more falls and injuries. Furthermore, the impact of age on hip replacement complications cannot be overstated. Older patients typically have less muscle mass and strength, and thus, are less able to compensate for the change in leg length. This can exacerbate the issue, leading to increased pain, discomfort, and possible need for additional corrective surgeries. Thus, it is critical to consider the potential for changes in leg length during the hip replacement process.
Dislocation Risks in Hip Replacement Procedures
Experiencing a hip dislocation is one of the potential complications that can arise after undergoing a hip replacement procedure. This serious consequence occurs when the ball of the artificial joint slips out of the socket. Preventing dislocation is a crucial component of post-operative care and involves specific movement restrictions, use of supportive devices, and physical therapy. Managing hip replacement pain is equally important, as discomfort can lead to involuntary movements that increase the risk of dislocation. Adequate pain management strategies involve a mix of medications, rest, and gentle exercises. Despite these measures, it's important to understand that certain activities or falls can still lead to dislocation, necessitating immediate medical attention.
Fractures as a Complication of Hip Replacement
During the period following a hip replacement surgery, fractures can emerge as a significant complication. These fractures, referred to as periprosthetic fractures, can occur around the hip implant, leading to pain and instability. The risk of such fractures can be accentuated in patients experiencing osteolysis, a condition characterized by bone loss. Prevention of periprosthetic fractures involves regular monitoring of the patient's bone health and minimizing risk factors such as falls. Osteolysis treatment options also play a crucial role in managing this complication. These include medication to slow down bone resorption, surgery to remove loose particles, or a complete revision surgery, if necessary. Implementing these preventive measures and treatment options can reduce the risk of fractures, enhancing the longevity and success of hip replacements.
The Dangers of Metallosis in Metal-on-Metal Hip Replacements
The phenomenon of Metallosis represents a significant risk in the realm of metal-on-metal hip replacements, characterized by an accumulation of metallic debris in the body's soft tissues. This condition occurs when the friction between the components of metal on metal hip implants causes metallic particles to wear off and infiltrate the body, leading to metal poisoning complications. Over time, these particles can cause inflammation, tissue necrosis, and even bone deterioration surrounding the implant. Severe cases of metallosis can lead to implant failure, necessitating revision surgery. Patients may experience symptoms such as joint pain, difficulty walking, and swelling around the hip area. Ensuring regular follow-ups and blood tests for metal ion levels can aid in the timely detection of metallosis.
Tissue Damage: A Serious Complication of Hip Replacement
Significant tissue damage often manifests as a severe complication following hip replacement surgery, leading to prolonged recovery and, in some cases, additional surgical interventions. This damage typically arises when metallic debris from the implant accumulates in the body, triggering an inflammatory response that can lead to tissue death. Metallosis prevention is crucial in mitigating this risk. This can be achieved through careful selection of implant materials and regular post-operative monitoring. When osteolysis, or bone loss, occurs due to this inflammation, treatment options such as medication to slow bone resorption, or in severe cases, revision surgery, may be necessary. Understanding and addressing these complications is essential to improving patient outcomes after hip replacement.
The Legal Aspects of Hip Replacement Complications
As we delve into the legal aspects of hip replacement complications, it is crucial to understand that patients may have legal recourse if they suffer from severe complications associated with their hip implant. If a patient experiences surgical complications, device failure, or any other related issue, they should consider potential legal action. This can hold manufacturers accountable and help victims obtain compensation for their injuries. There are various compensation options available, including settlement for medical expenses, loss of earnings, pain and suffering. Legal action also plays a significant role in prompting changes in the medical device industry, thus protecting future patients. However, understanding the legal process related to hip replacement complications often requires the advice of experienced legal professionals.
Risk Factors That Increase Hip Replacement Complications
While hip replacement surgery generally comes with the potential for complications, certain risk factors can ramp up the possibility of such issues and, concurrently, the severity of their impact on patients' health. Some patients may develop metallosis, a condition caused by the buildup of metallic debris in the body, often associated with metal-on-metal hip implants. The rates of metallosis have seen a decline with the decreased usage of such implants. Another complication, osteolysis, represents a significant risk factor. Osteolysis complications stem from the accumulation of debris from artificial hip wear, causing inflammation, bone destruction, and loosening of the hip implant. The combination of these risk factors can lead to severe complications, making patient selection and post-operative care essential.
The Long-Term Effects of Hip Replacement: The Issue of Wear
Understanding the long-term effects of hip replacement requires a comprehensive examination of wear-related complications, a critical aspect of patient care in post-operative scenarios. Over time, the artificial hip joint can degrade due to regular use, resulting in wear and tear. Preventing wear is of paramount importance, as it can significantly influence the longevity of the implant, and thus, the quality of life for the patient. In some cases, wear particles can trigger a destructive process called osteolysis, a leading cause of implant failure. Managing osteolysis, therefore, becomes crucial in ensuring the success of hip replacements. This involves regular monitoring to detect early signs of wear and osteolysis, allowing for prompt intervention and possible revision surgery, if necessary.
The Threat of Metallosis in Hip Replacement
Among the many complications associated with hip replacements, one particularly severe issue is metallosis, a condition that affects a small but significant number of patients and can lead to serious health consequences. Metallosis occurs when metallic debris from the implant accumulates in the body, causing tissue death around the artificial hip and implant loosening. Metallosis treatment typically involves revision surgery to replace the problematic metal-on-metal implant. Prevention strategies for osteolysis, a related condition causing bone destruction, include the use of non-metallic implants and regular monitoring for early detection. Although rare, the threat of metallosis underscores the importance of informed decision-making and careful post-operative monitoring in hip replacement patients.
Osteolysis: A Severe Long-Term Complication of Hip Replacement
Remarkably, osteolysis has emerged as a significant long-term complication following hip replacement, often leading to serious bone damage and implant failure. This condition arises due to the gradual accumulation and reaction to microscopic debris from the implant, triggering chronic inflammation that dissolves the surrounding bone. As a result, the implant may loosen and require revision surgery. Preventing osteolysis involves regular monitoring and early detection through imaging techniques, as well as the use of advanced implant materials and designs that minimize debris production. In tandem, managing metallosis - another major factor contributing to osteolysis - is crucial. This involves the careful selection of implant materials, particularly avoiding metal-on-metal designs, and frequent monitoring of metal ion levels in the bloodstream.
Periprosthetic Fractures: A Potential Danger of Hip Replacement
In the realm of hip replacement complications, periprosthetic fractures pose a significant risk, often occurring years post-surgery and potentially leading to implant failure. These fractures are the result of trauma to the bone surrounding the prosthesis, and their likelihood is increased by conditions such as osteoporosis. Furthermore, long-term effects of metallosis and osteolysis can contribute to the incidence of periprosthetic fractures. Metallosis, a buildup of metallic debris, and osteolysis, the destruction of bone due to wear debris, both weaken the bone-implant interface. This weakening can lead to implant loosening or failure, necessitating additional surgery. Thus, while hip replacements can greatly improve quality of life, the potential for periprosthetic fractures underscores the importance of careful post-operative care and monitoring.
The Risk of Mortality After Hip Replacement Surgery
Approximately 0.29% of patients in the U.K. experienced mortality following hip replacement surgeries in 2011, representing a significant decrease from the 0.56% reported in 2003. This reduction can be attributed to advancements in surgical techniques, anesthesiology, and metallosis prevention. Metallosis, a condition caused by the buildup of metallic debris, has been a significant concern in hip replacement surgeries. However, the decline in hip replacement mortality rates indicates that preventive measures against metallosis and other complications are proving effective. It is crucial to continue efforts in reducing these rates further. This includes thorough patient screening, careful surgical execution, and diligent post-operative care, all of which play a critical role in the overall mortality risk after hip replacement surgery.
Frequently Asked Questions
What Are the Psychological Effects of Hip Replacement Complications on Patients?
The psychological effects of complications from medical procedures can significantly impact a patient's wellbeing. Emotional resilience is crucial in managing these effects, as it aids in coping with stress and adversity. Anxiety management is also important, as complications can induce feelings of worry and fear. Specifically, hip replacement complications can lead to feelings of frustration, depression, or fear of re-surgery, highlighting the necessity for psychological support during the recovery process.
How Can Patients Minimize the Risk of Complications Following a Hip Replacement Surgery?
To minimize the risk of complications following a hip replacement surgery, patients can engage in adequate pre-surgery preparation, which includes maintaining a healthy lifestyle and strengthening their muscles. Post-operation nutrition also plays a crucial role in recovery. Consuming a balanced diet rich in protein, vitamins, and minerals can speed up the healing process. It's also essential to follow the surgeon's instructions, including taking prescribed medications and attending all follow-up appointments. Regular physical therapy is also recommended.
Are There Any Alternative Treatments to Hip Replacement That Carry Fewer Risks?
Yes, there are alternatives to hip replacement that may carry fewer risks. Non-surgical remedies such as physical therapy, pain management, and lifestyle modifications can often effectively manage hip joint issues. Additionally, prosthetic innovations like hip resurfacing involve less bone removal and may pose less risk than total hip replacement. However, the suitability of these alternatives depends on the patient's individual health condition and the severity of their hip joint deterioration.
How Does Rehabilitation After Hip Replacement Surgery Impact the Likelihood of Complications?
Rehabilitation after hip replacement surgery plays a crucial role in reducing complications. Effective rehabilitation techniques, including physical therapy and exercises, improve joint mobility and strengthen muscles around the hip, thereby minimizing the risks of dislocation and fractures. Furthermore, post-surgery nutrition aids in tissue healing and boosts overall recovery. Thus, a comprehensive rehabilitation plan, coupled with a balanced diet, can significantly impact the patient's recovery trajectory and decrease the likelihood of postoperative complications.
What Is the Impact of Hip Replacement Complications on a Patient’s Quality of Life?
The impact of hip replacement complications on a patient's quality of life can be significant. Complication prevention is crucial to minimize these risks. Post-surgery nutrition plays a vital role in recovery and reducing the likelihood of complications. A well-balanced diet aids in healing, strengthens the immune system, and helps maintain a healthy weight, reducing stress on the new joint. However, complications can lead to prolonged pain, limited mobility, and additional surgeries, adversely affecting a patient's wellbeing.
Conclusion
In conclusion, hip replacement, while greatly enhancing life quality, carries potential complications. From joint loosening to metallosis, the risks vary in severity. Factors such as age, health, and lifestyle influence these outcomes. Acknowledging these risks allows patients to make informed decisions. As Hippocrates wisely stated, "Desperate times call for desperate measures." However, understanding the stakes can prevent desperation from leading to unforeseen consequences, thereby guiding patients towards a healthier tomorrow.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.