Hyperthyroidism Causes Unrelated to AFFF Exposure
We acknowledge that hyperthyroidism has a variety of causes unrelated to AFFF (Aqueous Film Forming Foam) exposure. Genetic predispositions, including specific mutations, play a significant role, alongside autoimmune thyroid diseases like Graves' disease. Equally, both iodine intake levels—whether excessive or deficient—and environmental toxins, including heavy metals and pesticides, contribute to hyperthyroidism risk. Additionally, certain syndromes and conditions can lead to an overactive thyroid, independent of chemical exposures. Understanding these factors is essential for managing and treating thyroid disorders effectively. Exploring these causes offers insights into more accurate diagnosis and tailored treatment strategies, guiding us towards better health outcomes.
Key Takeaways
- Genetic mutations in specific genes can increase susceptibility to autoimmune thyroid diseases, leading to hyperthyroidism.
- Excessive or deficient iodine intake can disrupt normal thyroid function, resulting in hyperthyroidism.
- Exposure to environmental toxins such as heavy metals and pesticides can interfere with thyroid hormone regulation.
- Autoimmune thyroid diseases like Graves' disease cause an overproduction of thyroid hormones, independent of AFFF exposure.
- Certain genetic syndromes, including Type II autoimmune polyendocrine syndrome, can predispose individuals to hyperthyroidism.
Genetic Predispositions
Throughout generations, genetic predispositions have greatly influenced our susceptibility to hyperthyroidism, shaping how we comprehend and treat this thyroid disorder. It's become evident that mutations in specific genes play an essential role in predisposing individuals to autoimmune thyroid diseases, such as Graves disease, which is a prevalent cause of hyperthyroidism. Additionally, Type II autoimmune polyendocrine syndrome, which is linked to genetic factors, increases the risk of developing hyperthyroidism.
Recent advances in genome-wide association studies have been instrumental in identifying specific genes associated with thyrotoxicosis. These studies have provided us with a clearer picture of the genetic underpinnings of hyperthyroid conditions, allowing for a more nuanced understanding of why certain individuals are more susceptible to these disorders. It's fascinating how these genetic markers can now contribute to personalized treatment strategies, tailoring interventions to the unique genetic makeup of each individual suffering from hyperthyroidism.
Understanding these genetic predispositions is not just about identifying risks but also about crafting more effective and targeted treatment plans. By pinpointing the mutations and genetic factors that contribute to the development of autoimmune thyroid diseases like Graves disease and Type II autoimmune polyendocrine syndrome, we're moving towards a future where treatment for hyperthyroidism can be more precisely aligned with an individual's genetic profile. This approach holds the promise of improving outcomes for those affected by hyperthyroidism, reducing the trial and error often associated with managing this complex thyroid disorder.
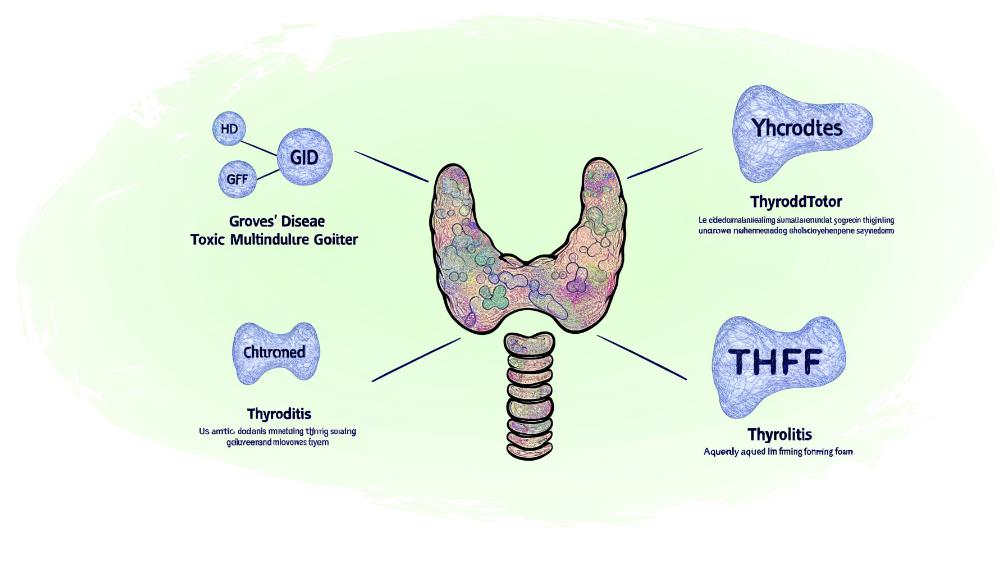
Autoimmune Thyroid Disease
Autoimmune thyroid diseases, such as Graves' disease and Hashimoto's thyroiditis, are key factors in the development of hyperthyroidism, stemming from our body's immune system mistakenly attacking the thyroid gland. While Graves' disease leads to the overproduction of thyroid hormones due to autoantibodies stimulating the thyroid, Hashimoto's thyroiditis often results in hypothyroidism, with the immune system damaging the thyroid and impairing hormone production. We've come to understand that these conditions are not only prevalent but are also significant contributors to thyroid dysfunction, unrelated to environmental factors like AFFF exposure.
These autoimmune thyroid diseases are complex, influenced by a mix of genetic predisposition, environmental factors, and immune system dysfunction. It's fascinating to see how our body's defense mechanisms, designed to protect us, can sometimes go awry, leading to these conditions. The autoimmune response triggers an imbalance in hormone levels, which can have widespread effects on our health.
Managing these diseases involves a careful balance of treatments aimed at regulating hormone levels and, in some cases, addressing the underlying autoimmune response. This might include medication to control hyperthyroidism in Graves' disease or hormone replacement in the case of Hashimoto's-induced hypothyroidism. It's a delicate dance to restore and maintain normal thyroid function and make sure individuals can lead healthy lives despite their autoimmune conditions.
Understanding the interplay between genetic factors, immune system dysfunction, and environmental influences helps us better manage and treat these diseases. It's clear that while we've made strides in understanding autoimmune thyroid disease, there's still much to learn about preventing and treating these complex conditions effectively.
Iodine Intake Levels

While we've explored how our immune system can mistakenly attack the thyroid, another significant factor in thyroid health is the role of iodine intake. Adequate iodine intake is essential for thyroid hormone synthesis and normal thyroid function. Without it, the body cannot produce enough thyroid hormones, leading to various health issues.
On the flip side, excessive iodine intake can also lead to complications, such as hyperthyroidism, especially in vulnerable populations. This condition, where the thyroid gland is overactive, producing too much hormone, can be as much a concern as its deficiency. It's a delicate balance that requires careful monitoring of iodine levels in our diet to prevent thyroid disorders, including hyperthyroidism.
Iodine deficiency is a prevalent cause of goiter, an enlargement of the thyroid gland, and can contribute to the development of hyperthyroidism. To combat this, the World Health Organization recommends a daily iodine intake of 150 micrograms for adults. This guideline is set to help prevent thyroid disorders and ensure that the population maintains adequate iodine levels for peak thyroid health.
Therefore, monitoring iodine levels is essential. It's not merely about preventing iodine deficiency but also about avoiding excessive intake that could trigger hyperthyroidism and other thyroid-related issues. Especially among vulnerable populations, keeping an eye on dietary iodine intake is imperative for maintaining thyroid health and preventing disorders. By adhering to recommended daily intake levels and monitoring our iodine consumption, we can safeguard our thyroid health and prevent the myriad of issues associated with its imbalance.
Environmental Toxins
Many environmental toxins, including heavy metals and pesticides, can greatly contribute to the development of hyperthyroidism by disrupting normal thyroid function. These substances, pervasive in our environment, pose significant risks not only to our ecosystem but also to our health. Among the culprits, polychlorinated biphenyls (PCBs) and dioxins stand out as industrial pollutants with a notorious reputation for affecting thyroid hormone regulation. Despite being banned or restricted in many parts of the world, their lingering presence in the environment continues to pose a threat.
Moreover, endocrine-disrupting chemicals, which interfere with the body's hormone systems, have been identified as a major concern. These chemicals, which include some pesticides and heavy metals, can mimic thyroid hormones or block their action, leading to a cascade of hormonal imbalances culminating in hyperthyroidism. The mechanism through which these environmental toxins affect thyroid function highlights the intricate interplay between external substances and our internal hormonal regulation.
The risk of developing hyperthyroidism increases with prolonged exposure to these environmental toxins. Continuous interaction with these pollutants, often through contaminated water, air, and food, magnifies their impact on our thyroid health. It's important to recognize the role that these environmental factors play in thyroid disorders, as they underline the significance of maintaining a clean and safe environment to protect not only our thyroid health but our overall well-being.
Specific Syndromes
Beyond environmental toxins, specific genetic syndromes also greatly contribute to the occurrence of hyperthyroidism. It is vital to recognize that conditions like Turner syndrome, a genetic disorder affecting females, can lead to hyperthyroidism without any connection to AFFF exposure. Similarly, Type II autoimmune polyendocrine syndrome, which is linked to hyperthyroidism, occurs independently of such environmental factors. We've also identified McCune-Albright syndrome among the syndromes that can cause hyperthyroidism, clearly demonstrating that AFFF exposure isn't the only risk factor.
Genetic factors and mutations are at the heart of many thyroid disorders, including hyperthyroidism. These genetic influences can significantly increase the risk of developing thyroid problems, irrespective of environmental toxin exposure. For instance, certain mutations can lead to a heightened sensitivity or response within the thyroid gland, contributing to hyperthyroidism. It is crucial to understand the genetic underpinnings that predispose individuals to thyroid disorders.
Moreover, iodine intake levels play a critical role in the development of hyperthyroidism. Whether too high or too low, iodine levels can impact thyroid function, leading to hyperthyroidism in some cases. This is a factor that operates independently of any external chemical exposure, including AFFF.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.




