Hysterectomy
You might find it surprising that over 600,000 hysterectomies are performed in the United States each year, making it one of the most common surgeries among women. As you're considering whether this procedure is the right choice for you, it's crucial to weigh the immediate and long-term impacts it might have on your health and lifestyle. From understanding the various types of hysterectomies to evaluating alternative treatments and managing post-surgery recovery, there's a lot to consider. Let's explore why this decision requires a comprehensive look beyond the surgery itself, ensuring you're fully informed about what to expect and how it could affect your life.

Types of Hysterectomies
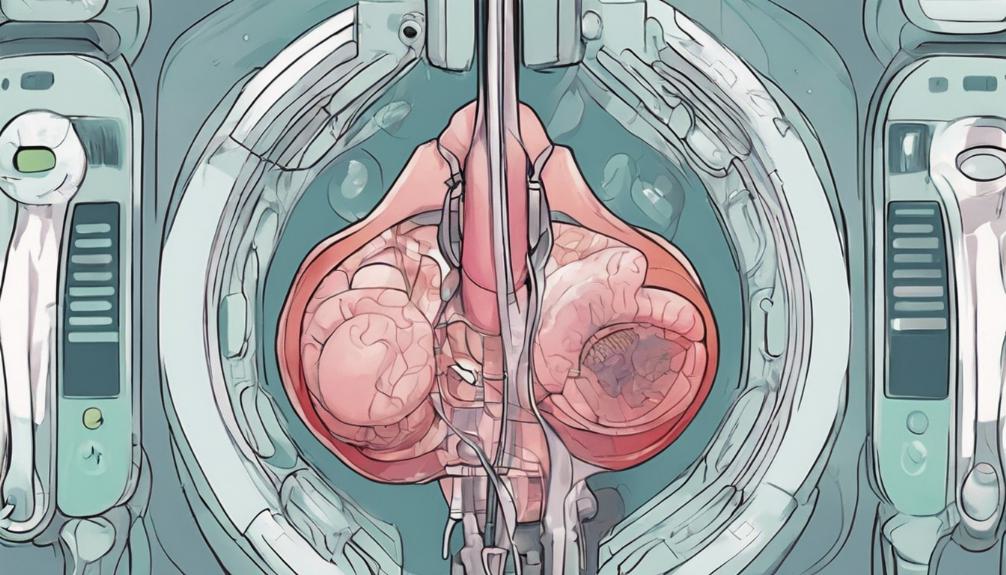
Understanding the different types of hysterectomies can help you make an informed decision about your healthcare options. If you're considering this surgery, it's crucial to know what each type entails. A total hysterectomy involves removing your entire uterus, offering a solution when conditions affect the whole uterus. In contrast, a partial hysterectomy, also called a supracervical hysterectomy, removes just the upper part of your uterus, leaving your cervix in place. This option might suit you if your condition is confined to the upper uterus. The most extensive, a radical hysterectomy, is typically for cancer treatment, removing the uterus, cervix, and surrounding tissue. Each type has different implications for recovery and future health, so you'll want to weigh these carefully with your doctor.
Reasons for Undergoing Hysterectomy

Several conditions may lead you to consider a hysterectomy, including uterine fibroids that cause pain and heavy bleeding. If you're experiencing severe menstrual bleeding possibly due to hormonal imbalances, infections, or even cancer, a hysterectomy might be on your horizon. Uterine prolapse, where your uterus slips into the vaginal canal, causing discomfort and issues with urination and bowel movements, is another significant reason. Moreover, endometriosis, with its debilitating pain and abnormal bleeding, and adenomyosis, causing intense pain and heavy periods, are conditions that often lead to this surgical decision. These issues not only affect your physical health but can deeply impact your quality of life, leading to the consideration of a hysterectomy as a viable solution.
Alternative Treatments

Before considering a hysterectomy, you might explore various alternative treatments tailored to your specific condition. If you're grappling with uterine fibroids, watchful waiting is often a first step, giving your body time to adjust naturally. For those experiencing uterine prolapse, Kegel exercises can strengthen pelvic muscles, and a vaginal pessary might offer support to hold organs in place. If endometriosis is your concern, medications can manage symptoms, reducing pain and bleeding. Each alternative aims to address your symptoms with less invasive approaches. It's crucial to discuss these options with your doctor, weighing the benefits against potential risks. Remember, the path you choose should align with your health goals and lifestyle.
Surgical Considerations
When considering a hysterectomy, it's crucial to weigh the surgical options available to you. You've got several paths, each with its own set of benefits and considerations. If you're looking at reducing recovery time, minimally invasive procedures like laparoscopic or robotic surgery might be your best bet. They use smaller incisions, leading to less pain and a quicker return to your daily activities. However, not everyone's a candidate for these methods. Your condition, overall health, and the size of your uterus play a big role in determining the suitable approach. It's also important to discuss with your doctor whether you'll be keeping your ovaries, as this decision impacts hormonal balance post-surgery. Remember, the goal is to choose the option that aligns with your health needs and recovery expectations.
Abdominal Hysterectomy Explained

An abdominal hysterectomy, one of the more common surgical methods, involves making a significant incision in your lower abdomen to remove the uterus. This procedure might be recommended if you're experiencing severe conditions like large uterine fibroids, cancer, or significant pelvic pain due to various gynecological issues. Depending on your health and the reason for the surgery, your doctor might remove the entire uterus or just a part. It's a major operation, requiring a hospital stay and a recovery period that spans several weeks. You'll need to take it easy, avoiding strenuous activities to allow your body to heal properly. It's crucial to follow your doctor's aftercare instructions closely to minimize the risk of complications and ensure the best possible recovery.
Vaginal Hysterectomy Procedure
In a vaginal hysterectomy, your surgeon removes your uterus through a small incision made inside your vagina, offering a less invasive alternative to the traditional abdominal method. This approach means you'll likely experience less pain post-surgery and enjoy a faster recovery time. You're a good candidate if you have a non-enlarged uterus and conditions like uterine prolapse or fibroids that haven't grown too large.
The procedure typically lasts one to two hours, and you can expect to stay in the hospital for at least one night. Recovery involves resting and avoiding heavy lifting for about four to six weeks. You'll need to follow up with your doctor to ensure healing is progressing well. Remember, it's crucial to discuss all your options and understand the procedure's implications fully before moving forward.
Laparoscopic Hysterectomy Overview
Exploring another less invasive option, laparoscopic hysterectomy involves making small incisions in the abdomen for the removal of the uterus. You'll find this method particularly appealing if you're aiming for a quicker recovery time with less scarring. Unlike traditional surgeries, your surgeon uses a laparoscope—a thin, lighted tube with a camera—to guide the procedure through these small cuts, removing the uterus with precision tools. You're likely to appreciate the minimal hospital stay and the reduced discomfort post-surgery. It's a solid choice if you're facing conditions like fibroids, endometriosis, or uterine prolapse. Remember, it's crucial to discuss all your options thoroughly with your doctor to ensure this method suits your medical and personal needs.
Robotic Surgery Insights
Delving into robotic surgery, you'll discover a cutting-edge option that offers precision and flexibility beyond traditional methods. This approach utilizes robotic arms, controlled by a surgeon through a console, to perform the hysterectomy with remarkable accuracy. You're looking at smaller incisions, which translates to less pain and a quicker recovery time compared to open surgery. The robotic arms can rotate and bend far beyond the capabilities of the human hand, allowing for meticulous dissection and suturing. This method is particularly beneficial if you're facing complex conditions where precision is paramount. Remember, while the benefits are significant, it's crucial to discuss with your doctor whether this innovative approach aligns with your specific medical needs and personal circumstances.
Hospital Stay and Aftercare

After your hysterectomy, you'll typically spend 1 to 2 days in the hospital to start your recovery process. During this time, you'll be closely monitored to ensure your pain is managed and that there are no complications from the surgery. Nurses will encourage you to walk around as soon as possible to prevent blood clots and speed up your recovery. You'll also learn how to care for your incision site, which is crucial to prevent infection.
Before you leave the hospital, your healthcare team will provide detailed aftercare instructions. This includes advice on managing pain, recognizing signs of potential complications, and scheduling follow-up appointments. They'll also guide you on activity restrictions to avoid straining your incision site. Remember, this hospital stay is just the beginning of your healing journey.
Recovery and Healing

Embarking on the recovery and healing process, you'll find that your body gradually regains strength and normalcy following the hysterectomy. It's crucial to follow your doctor's advice closely, ensuring you give yourself the rest needed. You'll be encouraged to walk around as soon as possible to prevent blood clots and improve circulation, but remember, no heavy lifting or strenuous activity for at least 4-6 weeks. It's normal to experience some fatigue and discomfort during this time, so don't hesitate to ask for pain relief if needed. Keep a lookout for any signs of infection around your incision sites and maintain a healthy diet to support your healing. With patience and proper care, you're on your way to recovery.
Post-Hysterectomy Symptoms

Following a hysterectomy, you may notice various changes and symptoms as your body adjusts. It's common to experience a range of physical sensations. Initially, you'll likely deal with some abdominal pain and swelling. This discomfort is your body's way of healing. You might also face changes in your bowel movements and urinary habits, including constipation or difficulty emptying your bladder fully.
As your hormones adjust, especially if your ovaries were removed, you could start experiencing symptoms of menopause, such as hot flashes and night sweats, sooner than you might have naturally. It's crucial to keep in touch with your healthcare provider about these changes. They can offer strategies to manage these symptoms effectively, ensuring a smoother transition during your post-hysterectomy recovery.
Emotional and Sexual Well-being

While adjusting to the physical changes post-hysterectomy, it's also vital to consider your emotional and sexual well-being. You might experience a range of emotions, from relief to sadness or loss. It's normal to feel a mix of these emotions, and talking to a therapist or joining a support group can help you navigate through them.
Sexual well-being is also an important aspect to address. You may notice changes like vaginal dryness, which can affect your intimacy. Don't shy away from exploring solutions with your partner and healthcare provider. Lubricants or hormonal treatments might offer relief. Remember, it's possible to maintain or even improve your sexual life post-surgery. Open communication with your partner and seeking professional advice are key steps to ensuring your emotional and sexual well-being.
Ongoing Health Screenings

After undergoing a hysterectomy, it's crucial to keep up with ongoing health screenings to monitor your overall well-being. You're not off the hook for regular check-ups, even if you've had your uterus removed. Depending on the type of hysterectomy and whether your ovaries were left intact, you'll still need screenings for ovarian and breast cancer. Pap tests may no longer be necessary if your cervix was removed, but you should discuss this with your doctor. Don't forget about heart health and bone density tests, as you're at an increased risk for cardiovascular disease and osteoporosis post-hysterectomy, especially if you've entered menopause earlier than expected. Staying vigilant with these screenings helps catch potential health issues early, ensuring you maintain the best health possible.
Frequently Asked Questions
How Does a Hysterectomy Affect Long-Term Hormone Levels and Do I Need Hormone Replacement Therapy (Hrt) After the Surgery?
After your surgery, your long-term hormone levels might drop, especially if your ovaries are removed. This can lead you into menopause sooner than expected. Whether you'll need hormone replacement therapy (HRT) depends on your symptoms, age, and overall health. It's crucial to discuss this with your doctor, who can tailor advice to your specific needs. HRT can help manage menopause symptoms, but it's not suitable for everyone.
Can a Hysterectomy Impact My Ability to Lose Weight or Change My Metabolism in Any Significant Way?
If you're worried about weight loss or metabolism changes post-surgery, it's a valid concern. Your body's response can vary. Some people notice changes in their metabolism or struggle with weight management after major surgeries. It's due to shifts in physical activity levels, changes in hormone balance, and recovery processes. Staying active and maintaining a healthy diet are key. Yet, specific effects depend on individual health conditions and the type of procedure undergone.
What Are the Specific Risks Associated With Undergoing a Hysterectomy Later in Life, Particularly Post-Menopause?
If you're considering surgery later in life, especially after menopause, you're facing unique risks. These can include a higher chance of complications like infections, bleeding, or reactions to anesthesia. Your recovery might also take longer, impacting your return to daily activities. It's crucial to weigh these risks against the potential benefits and discuss them thoroughly with your doctor to make an informed decision that's right for you.
Are There Any Natural or Alternative Remedies Recommended for Managing Post-Hysterectomy Symptoms, Especially for Those Who Prefer Not to Use Traditional Medication?
If you're seeking natural remedies to manage symptoms after a significant surgery, you've got options. Kegel exercises can strengthen pelvic muscles, easing discomfort. A balanced diet, rich in phytoestrogens from soy and flaxseed, might alleviate menopausal symptoms. Acupuncture and yoga can reduce stress and pain. Herbal supplements like black cohosh may help, but always check with your doctor first. Staying hydrated and regular physical activity can also improve your overall well-being.
How Does a Hysterectomy Affect One's Risk of Developing Osteoporosis or Cardiovascular Diseases, and What Preventive Measures Can Be Taken?
You're curious about the link between surgical procedures and your risk for osteoporosis or cardiovascular diseases, and what you can do to prevent these conditions. Removing your uterus can impact hormone levels, potentially increasing your risk for these health issues. To counteract this, you should focus on a healthy diet, regular weight-bearing exercise, and possibly hormone replacement therapy. It's also crucial to monitor your bone density and heart health closely with your doctor.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.




