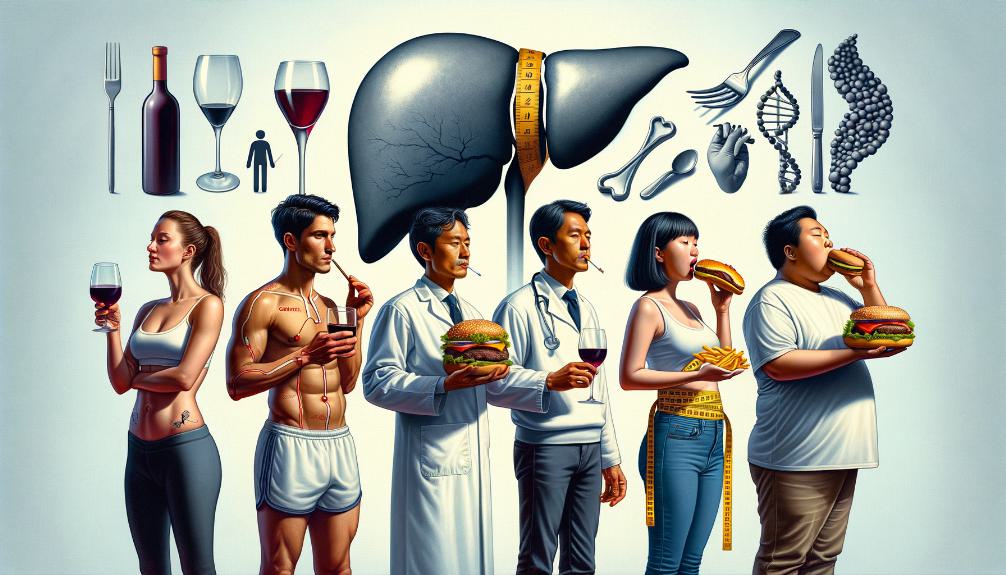
Liver Cancer Risk Factors Unrelated to AFFF
We've determined that liver cancer risk factors not linked to Aqueous Film-Forming Foams (AFFF) span a wide range, from lifestyle habits to genetic predispositions. Diets high in processed meats, low fruit and vegetable intake, obesity, and a sedentary lifestyle greatly elevate risks. Chronic viral infections like hepatitis B and C, certain genetic mutations, along with exposure to environmental toxins such as industrial chemicals, have been identified as key contributors. Additionally, heavy use of alcohol and tobacco, alongside obesity and type 2 diabetes, heighten liver cancer dangers. By focusing on these areas, there's potential for targeted prevention and early intervention, paving the way for significant insights into mitigating liver cancer risks.
Key Takeaways
- Chronic viral infections like hepatitis B and C significantly increase liver cancer risk.
- Obesity and a sedentary lifestyle elevate the likelihood of developing liver cancer.
- Exposure to environmental toxins, including arsenic and cadmium, raises liver cancer risk.
- Genetic predispositions, such as mutations in BRCA1, BRCA2, and TP53 genes, heighten susceptibility.
- Alcohol and tobacco use are major contributors, with heavy drinking and smoking significantly raising liver cancer risk.
Lifestyle and Diet

Our lifestyle and diet play a crucial role in either increasing or decreasing the risk of liver cancer. We've learned that indulging in a diet high in processed meats and low in fruits and vegetables can greatly up our chances of developing this serious condition. It's not just about what we eat, but also our physical state. Being obese or overweight isn't just a matter of discomfort or aesthetics; it elevates our liver cancer risk by a striking 37% with every 5-unit increase in BMI.
Moreover, we can't ignore the impact of our beverage choices. Regularly downing sugary beverages and foods packed with added sugars is like setting the stage for liver cancer to make an entrance. It's concerning how these seemingly harmless daily choices can accumulate and lead to such severe consequences.
Let's not forget the role of physical activity, or the lack thereof, in this equation. Our sedentary lifestyles, marked by physical inactivity, are silently but significantly heightening our liver cancer risk. It emphasizes the critical need for regular exercise as a potent countermeasure.
Lastly, we can't overlook the damage caused by excessive alcohol consumption. As a modifiable risk factor, heavy alcohol use not only leads to liver-related diseases but also stands as a leading cause of liver cancer.
In light of these facts, it's clear we have considerable control over our liver cancer risk through our lifestyle and dietary choices. Making conscious decisions to exercise regularly, moderate our alcohol intake, and opt for a diet rich in fruits and vegetables over processed meats and sugary beverages can be a life-saving shift.
Chronic Viral Infections
Among the most significant risk factors for liver cancer, chronic viral infections like hepatitis B and C stand out, affecting millions worldwide. These infections, primarily caused by the hepatitis B virus (HBV) and hepatitis C virus (HCV), are pivotal in the landscape of liver cancer risk factors. It's important to understand that chronic viral hepatitis, due to these viruses, can lead to liver cirrhosis, a condition that markedly increases the risk of developing liver cancer.
Chronic infections with HBV or HCV are not merely health concerns but are significant contributors to the global burden of hepatocellular carcinoma, the most common type of primary liver cancer. This relationship underscores the importance of addressing chronic viral infections as a pathway to reducing liver cancer cases. It's evident that these chronic viral infections play a central role in the mechanism of liver cancer development, drawing a direct line from infection to potential cancer diagnosis.
The connection between chronic viral hepatitis and liver cancer emphasizes the necessity of effective treatment and management of these infections. By tackling HBV and HCV with thorough treatment strategies, we're not just fighting the infections themselves but are actively working to decrease the likelihood of liver cancer development. This approach is crucial in the global health strategy to reduce liver cancer cases and improve patient outcomes.
Understanding the link between chronic viral infections and liver cancer development is a critical step in mitigating the impact of liver cancer worldwide. Through effective treatment of HBV and HCV, we're not only addressing immediate health concerns but are also taking significant strides in preventing liver cancer, a prevalent and serious health challenge.
Genetic Predispositions

Turning our attention to genetic predispositions, we must acknowledge that familial patterns of liver cancer and the identification of specific genetic mutations play a significant role in understanding risk factors. These elements highlight the importance of looking beyond environmental and lifestyle influences to grasp the full spectrum of liver cancer risks. By focusing on genetic markers and hereditary trends, we're able to offer more personalized and effective strategies for prevention and management.
Familial Liver Cancer Patterns
We'll explore how familial liver cancer patterns reveal a genetic predisposition, putting certain families at higher risk of developing the disease. These patterns, underscored by inherited genetic mutations such as BRCA1, BRCA2, APC, and TP53, greatly elevate the risk of liver cancer. Conditions like hereditary hemochromatosis and Wilson's disease are closely associated with liver cancer development. Additionally, Lynch syndrome and familial adenomatous polyposis (FAP) are linked to a higher risk of liver cancer. Understanding these familial liver cancer patterns is vital in identifying individuals at elevated risk. This insight allows for targeted monitoring and early intervention, aiming to mitigate the impact of liver cancer among predisposed families.
Genetic Mutations Identification
Exploring the domain of genetics, it is crucial to identify specific mutations that significantly increase the risk of liver cancer in individuals. Genetic mutations, especially in the TP53 gene, are closely linked to an elevated predisposition to liver cancer. Inherited conditions such as hereditary hemochromatosis and Wilson's disease further enhance this risk, highlighting a clear genetic component in the disease's etiology. Additionally, mutations in the CTNNB1 gene have been directly associated with hepatocellular carcinoma, the most prevalent form of liver cancer. Understanding these genetic predispositions through targeted testing can help pinpoint individuals at higher risk, while familial clustering of liver cancer cases underscores the importance of recognizing the genetic component in evaluating liver cancer risk.
Environmental Toxins
Shifting our focus to environmental toxins, we discover that they play a significant role in the development of liver cancer. Exposure to industrial chemicals, heavy metals, and pesticides has been linked to an increased risk of various forms of this disease. It's imperative that we comprehend how these substances, found in our everyday environment, contribute to the rising instances of liver cancer.
Industrial Chemical Exposure
Among the critical factors elevating the risk of liver cancer, exposure to industrial chemicals like vinyl chloride, arsenic, cadmium, and organic solvents stands out as particularly hazardous. These toxins, found in various workplaces, play a key role in the development of serious conditions such as liver angiosarcoma and hepatocellular carcinoma. Vinyl chloride, a key component in PVC production, along with arsenic and cadmium—naturally occurring metals—have been explicitly linked to hepatocarcinogenesis. Additionally, exposure to organic solvents and N-nitrosamines, prevalent in several industries, is acknowledged as carcinogenic. It's imperative that occupational exposure to these dangerous substances is minimized to reduce liver cancer risk, underscoring the importance of stringent safety standards and protective measures in the workplace.
Heavy Metal Contamination
Beyond industrial settings, we can't ignore the significant role that environmental toxins, such as arsenic and cadmium, play in elevating liver cancer risk. These heavy metals, known to be hepatocarcinogenic, are linked with a higher incidence of liver cancer. Exposure to these environmental toxins, especially through contaminated water or soil, underscores the necessity for vigilant monitoring and reducing our exposure levels. The association between heavy metal contamination and liver cancer risk is well-documented, highlighting the critical need to address these environmental toxins. Through improved monitoring and efforts to minimize exposure, we're taking essential steps towards lowering the risk of liver cancer. Understanding the impact of arsenic and cadmium exposure is pivotal in our fight against this disease.
Pesticide Usage Impact
We must also consider the significant impact that pesticide usage has on increasing the risk of liver cancer. Pesticides like DDT are recognized as possibly hepatocarcinogenic, indicating a potential contribution to the risk associated with liver cancer. The exposure to insecticides that harbor carcinogenic compounds can heighten the likelihood of this disease. In occupational settings, certain pesticides and herbicides are particularly linked to the development of liver cancer, emphasizing the role of occupational exposure in the assessment of risk factors. The chronic interaction with environmental toxins, including various pesticides, underscores a crucial concern for liver health across specific populations. Understanding how pesticide usage influences liver health is essential for implementing preventive measures against liver cancer, highlighting the importance of mitigating these environmental toxins.
Alcohol and Tobacco Use
Understanding the role of alcohol and tobacco use is vital in the battle against liver cancer, as these habits greatly increase the risk. It's concerning to note that alcohol consumption is linked to 7% of liver cancer cases in the UK, with heavy drinking considerably raising the likelihood of this disease. Similarly, smoking tobacco is not far behind, being responsible for 20% of liver cancer cases in the UK. This highlights the profound impact that tobacco use has on liver health.
The combustion of tobacco releases carcinogens like beta-naphthylamine and polycyclic aromatic hydrocarbons. These substances are known to elevate the risk of liver cancer, underscoring the dangers of smoking. Additionally, the International Agency for Research on Cancer (IARC) classifies tobacco as a group 1 carcinogen. This designation emphasizes tobacco's strong link to various forms of cancer, including liver cancer, and serves as a stark warning about the risks associated with tobacco use.
Furthermore, genetic polymorphisms can heighten susceptibility to liver cancer among smokers. This suggests that certain individuals may be more vulnerable to the harmful effects of tobacco on liver health due to their genetic makeup. It's essential, hence, for us to understand the role of alcohol and tobacco in liver cancer development. By recognizing these risk factors, we can take proactive steps to mitigate their impact and protect our liver health. Our collective effort in reducing heavy drinking and smoking can markedly lower the incidence of liver cancer, making a considerable difference in public health outcomes.
Obesity and Diabetes

While addressing alcohol and tobacco's role in liver cancer is important, we shouldn't overlook the substantial impact of obesity and diabetes on this condition. Studies have shown that obesity is linked to 23% of liver cancer cases in the UK, presenting a 37% higher risk for individuals with each 5-unit increase in BMI. This stark statistic underscores the critical need for weight management as a preventive measure against liver cancer.
Similarly, diabetes, particularly type 2 diabetes, is a modifiable risk factor that significantly contributes to the increased risk of liver cancer. Individuals with diabetes are at a higher risk of developing liver cancer compared to those without the condition, further highlighting the intertwined relationship between obesity and diabetes as risk factors for liver cancer. This connection emphasizes the urgent need for lifestyle modifications to mitigate these risks.
Given the prevalence of obesity and diabetes in the population, it's paramount that we advocate for regular screenings and encourage individuals to adopt healthier lifestyles. Such efforts can play a crucial role in reducing the number of liver cancer cases. By focusing on weight management and controlling diabetes, we can significantly lower the risk of liver cancer. This approach not only addresses the immediate concerns related to liver cancer but also contributes to the overall well-being of individuals, steering them away from other health issues associated with obesity and diabetes.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.




