Low Birthweight Causes in AFFF Cases: Beyond Exposure
We're investigating the complex factors contributing to low birthweight in AFFF cases, beyond PFAS exposure. Vital elements include maternal health impacts such as nutritional deficiencies and stress, which are exacerbated by AFFF exposure. These conditions not only elevate the risk of gestational diabetes but also hinder fetal development. Environmental contamination around military bases and airports further complicates these risks. Legal actions against AFFF manufacturers underscore the health hazards linked with exposure. Addressing these multifaceted issues requires a holistic approach, focusing on both maternal health and environmental safety. Our analysis reveals broader implications for affected families, offering them insights into potential legal redress and preventive measures.

Key Takeaways
- Maternal nutritional deficiencies can significantly contribute to low birth weight in infants.
- Stress during pregnancy, particularly if intensified by AFFF exposure, negatively impacts birth weight.
- Gestational diabetes and insulin resistance, risks increased by AFFF exposure, are linked to low birth weight.
- Critical exposure periods during early pregnancy, not just the level of exposure, impact birth weight outcomes.
- Genetic vulnerabilities and systemic health disparities, such as those faced by Black babies, influence sensitivity to AFFF contaminants and birth weight.
PFAS and Pregnancy

During pregnancy, exposure to PFAS can greatly increase the risk of babies being born with low birth weight. This is a concerning fact that we've come to understand, emphasizing the need for heightened awareness and action against PFAS exposure. Research has illuminated how PFAS, even in utero, can disrupt cell differentiation and metabolism. This isn't just about the immediate effects; it's about the profound, lasting all-encompassing effects these chemicals can have on an unborn child's development.
We've seen evidence suggesting that children, whose earliest moments were marred by PFAS exposure, may not only catch up in weight rapidly, often bypassing healthy benchmarks, but they're also more prone to developing obesity between the ages of two to five. This isn't a simple issue of weight; it's about the fundamental processes of growth and development being skewed from the start. The interference of PFAS with DNA methylation processes during prenatal development is a critical point of concern, impacting how cells differentiate and how the body regulates metabolism.
This pattern of rapid weight gain without corresponding height increases is alarming. It's indicative of a deeper, more all-encompassing issue tied to PFAS exposure during pregnancy - an issue that has lasting repercussions. The risk of obesity, driven by these early exposures, underscores the urgency of addressing PFAS contamination. The legacy of PFAS exposure isn't just seen in environmental damage, but in the lasting impact on the most vulnerable among us, our children, highlighting the need for a widespread and proactive approach to this pressing health and legal challenge.
Maternal Health Impacts
We're now turning our attention to the impacts of maternal health on low birthweight in AFFF cases, exploring how nutritional deficiencies, stress levels, and chronic conditions play vital roles. It's essential to understand how these factors, combined with exposure to AFFF containing PFAS, can compound the risks for both mothers and their infants. By examining these elements, we aim to highlight the significant health challenges and legal considerations that arise from such exposures.
Nutritional Deficiencies Impact
Importantly, maternal nutritional deficiencies can greatly influence the incidence of low birthweight in infants, especially when compounded by AFFF exposure. It is crucial to understand that inadequate intake of vital nutrients during pregnancy, heightened by AFFF exposure, plays a key role in low birthweight outcomes. These nutrient deficiencies in expecting mothers can disrupt fetal growth, subsequently increasing the risk factors associated with low birthweight in newborns. Additionally, AFFF exposure can worsen maternal health issues, leading to compromised nutrient transfer to the fetus and potentially resulting in low birthweight complications. Addressing these nutritional imbalances in mothers, alongside mitigating AFFF exposure, is vital in reducing the risk of low birthweight in infants, highlighting the importance of maternal health in infant development.
Stress Levels Influence
Understanding the profound impact of stress levels on maternal health reveals how AFFF exposure can greatly contribute to low birthweight in infants. High maternal stress, intensified by AFFF exposure, not only jeopardizes fetal development but also paves the way for adverse birth outcomes. The link between stress during pregnancy and the risk of delivering a low birthweight baby is undeniable. Psychological stress, a substantial factor affecting maternal health, can impede the baby's growth in utero, underscoring the necessity of addressing maternal stress to mitigate the impact of AFFF exposure effectively. By focusing on reducing psychological stress in expectant mothers, we can significantly lessen the detrimental effects of AFFF on birthweight, ensuring healthier outcomes for both mother and child.
Chronic Conditions Role
As maternal exposure to AFFF containing PFAS is associated with an increased risk of gestational diabetes and insulin resistance, it's essential to explore how chronic conditions play a substantial role in impacting maternal health and subsequently leading to low birthweight in infants. The presence of chronic conditions such as diabetes, exacerbated by PFAS exposure, can greatly affect the intrauterine environment, hindering fetal development and contributing to low birthweight outcomes. This association between chronic conditions resulting from PFAS exposure and low birthweight underscores the importance of understanding the maternal health impacts of these environmental contaminants. Therefore, addressing and mitigating PFAS exposure is critical in safeguarding maternal health and preventing adverse birth outcomes.
Environmental Factors
Turning our attention to environmental factors, we'll now explore how industrial pollutants, water contamination risks, and air quality concerns play pivotal roles in the incidence of low birthweight in AFFF cases. It's clear that contaminants like PFAS, prevalent in AFFF, not only persist in our environment but also pose significant threats to fetal health. We're committed to examining how these environmental exposures contribute to adverse pregnancy outcomes, emphasizing the need for stringent regulations and protective measures.
Industrial Pollutants Impact
Industrial pollutants, particularly AFFF containing PFAS, seep into the environment, contaminating soil and groundwater near airports and military bases with long-lasting consequences. PFAS from AFFF have a notorious persistence, remaining in the environment for years, leading to significant health risks for individuals exposed through occupational or environmental means. The exposure to these industrial pollutants isn't just a matter of immediate concern; it's an ongoing struggle against contamination that affects communities' well-being. Thankfully, efforts are underway to tackle AFFF contamination, with environmental cleanup initiatives aimed at mitigating the spread of PFAS pollutants. These steps are vital in addressing the adverse health effects linked to PFAS exposure and ensuring a safer environment for future generations.
Water Contamination Risks
Building on our understanding of AFFF's environmental impact, we'll now explore how water contamination poses significant risks to ecological and human health. PFAS exposure through drinking water is a major concern, stemming from AFFF contamination. These chemicals persist in water bodies, elevating the potential for human exposure significantly. Not only does water contamination by AFFF impact soil quality and groundwater, but it also exacerbates environmental risks. Runoff from contaminated areas can spread PFAS into water sources, harming aquatic ecosystems. Monitoring water contamination is vital to mitigate these risks to environmental health. We're committed to keeping an eye on these developments, understanding the importance of managing water contamination from AFFF to protect both the environment and public health.
Air Quality Concerns
We're now shifting our focus to how AFFF contamination raises significant air quality concerns due to the release of volatile organic compounds. AFFF-contaminated sites compromise air quality, with environmental factors like wind patterns affecting the spread of these contaminants. The inhalation of airborne particles poses respiratory risks to those nearby, highlighting the importance of air sampling and monitoring programs. These initiatives are essential for evaluating the extent of airborne contamination and safeguarding public health. Exposure to these contaminants doesn't only pose immediate health risks but can also impact long-term respiratory health. Hence, understanding the dynamics of airborne contamination at AFFF sites is crucial for addressing these environmental and health challenges effectively.
Fetal Development Risks
Concerning fetal development risks, exposure to AFFF contaminants during pregnancy can greatly enhance the likelihood of low birthweight in babies. These risks are closely linked to the presence of PFAS, a group of chemicals found in AFFF that are associated with several adverse health outcomes. When we explore the impact of AFFF contaminants on fetal development, we find a distressing pattern: infants exposed to these chemicals in utero may encounter significant growth challenges, not just in their infancy, but potentially extending into later stages of life.
The connection between AFFF contaminants and low birthweight is particularly concerning because it lays the groundwork for a myriad of health issues. Babies born with low birthweight have been shown to have a higher susceptibility to infections shortly after birth, alongside facing long-term complications that can affect their overall development and quality of life. What makes this situation even more alarming is the fact that these outcomes are not just hypotheticals; they are realities being faced by families exposed to PFAS through AFFF.
As we investigate the specifics of how AFFF exposure affects fetal development, it's clear that PFAS exposure is a significant contributing factor to infant health complications. These chemicals can interfere with normal fetal growth processes, leading to babies being born smaller than expected. This interference not only poses immediate health risks but also sets the stage for potential developmental and growth challenges as the child ages.
In light of these facts, the importance of understanding and mitigating the risks associated with AFFF contaminants cannot be overstated. Protecting infant health from the adverse effects of PFAS exposure is an urgent priority that calls for concerted efforts from all stakeholders involved.
Duration of Exposure
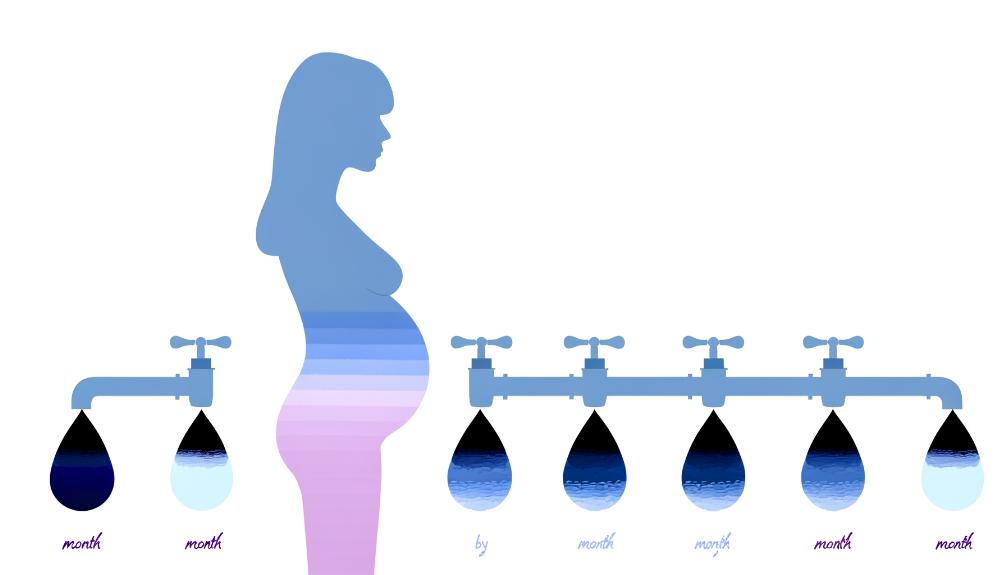
We've seen how exposure to PFAS in AFFF can disrupt fetal development, leading to low birthweight. Now, we'll turn our attention to how the length of exposure, specific critical periods, and the cumulative effects play a pivotal role in this process. Understanding these factors is essential for evaluating the risks and potential legal implications for affected families.
Exposure Length Impact
Regarding the impact of exposure length, it's clear that the longer individuals are exposed to AFFF containing PFAS compounds, the greater the risk of low birthweight in newborns. This connection between prolonged exposure to PFAS through AFFF and the negative impact on fetal growth and development cannot be overstated. Studies consistently show that extended exposure periods to these compounds markedly contribute to a higher likelihood of low birth weight. The duration of exposure plays a pivotal role in determining the severity of adverse effects on infant birth weight. Additionally, there's a cumulative effect to take into account; extended exposure to PFAS compounds from AFFF amplifies the risk of low birthweight in babies, underscoring the urgent need for addressing this critical issue.
Critical Exposure Periods
Understanding the critical exposure periods to AFFF contaminants during pregnancy is essential for grasping how these chemicals impact infant birthweight. Long-term exposure, particularly during early pregnancy, has been identified as a key period for potential adverse effects on birthweight. This finding underscores the importance of looking at specific exposure periods, or critical trimesters, that are most detrimental to fetal growth. The duration and timing of maternal exposure to AFFF contaminants are pivotal in influencing the likelihood of low birthweight outcomes in newborns. Prolonged exposure throughout gestation further compounds the risk, underscoring the need for careful monitoring of maternal exposure to AFFF pollutants to mitigate their impact on infant birthweight.
Cumulative Exposure Effects
The cumulative effects of prolonged exposure to AFFF's PFAS greatly elevate the risk of low birthweight in infants. It's become clear that not only the presence of PFAS but also the duration of exposure plays a pivotal role in this health crisis. The longer expectant mothers or their environments are exposed to AFFF, the higher the likelihood their babies will be born underweight. This is due to the cumulative exposure effects that interfere with fetal growth and development. Studies have consistently shown that extended exposure periods to PFAS from AFFF have a substantial impact on infant birth weight outcomes. This understanding underscores the critical need for addressing both the presence and the duration of exposure to mitigate the risks associated with low birthweight.
Nutritional Influences

Nutritional influences play a vital role in fetal growth, directly impacting birthweight outcomes. It's become increasingly clear that adequate maternal nutrition during pregnancy is not just beneficial but essential for the proper growth and development of the fetus, which in turn can greatly influence birthweight. Nutritional deficiencies, particularly in essential nutrients such as folic acid and iron, are known contributors to low birthweight. These deficiencies highlight the importance of a well-rounded and nutrient-rich diet during this critical period.
A poor maternal diet, lacking in these key nutrients, undeniably increases the risk of giving birth to infants with low birthweight. This risk underscores the necessity of consuming a balanced diet that supports both the mother's health and the developing fetus's needs. Additionally, nutritional interventions and thorough prenatal care have emerged as crucial components in preventing and addressing low birthweight cases, especially in infants exposed to AFFF.
Our focus on nutritional influences emphasizes the significance of maternal nutrition in fetal growth and development. Ensuring adequate nutrient intake through a balanced diet is essential, not just for the health and well-being of the mother but also for setting the foundation for the infant's health. Prenatal care, with a strong emphasis on nutritional guidance, plays a major role in mitigating the risk of low birthweight, demonstrating the interconnectedness of maternal health practices and ideal birthweight outcomes. Through these interventions, we're equipped to better manage and prevent the occurrence of low birthweight in infants, beyond just addressing exposure concerns.
Stress and Mental Health
While we've explored the impact of nutrition on fetal development, it's equally important to acknowledge how stress and mental health during pregnancy can significantly influence birthweight outcomes. The connection between stress and low birthweight is well-documented, emphasizing the significant role mental well-being plays in fetal development. High levels of stress during pregnancy, spurred by various factors, have been directly linked to lower birthweight in newborns, underscoring the need for effective stress management and mental health support for expectant mothers.
Maternal mental health disorders, including anxiety and depression, further compound the risk of low birthweight. These conditions not only affect the mother's quality of life but also have tangible impacts on the developing fetus. Chronic stress triggers hormonal changes that can adversely affect fetal growth, potentially leading to low birthweight. This highlights the critical importance of addressing mental health concerns during pregnancy as part of thorough prenatal care.
Fortunately, mental health interventions like therapy and counseling have shown promise in mitigating these risks. By reducing stress levels in pregnant individuals, these interventions can play a key role in preventing low birthweight outcomes. It's clear that tackling maternal stress and mental health issues is a vital step in safeguarding fetal development and ensuring healthier birthweight outcomes.
Therefore, our focus must extend beyond traditional prenatal care to include robust support for mental health and stress management. This all-encompassing approach is essential in preventing complications associated with low birthweight and improving overall pregnancy outcomes.
Prenatal Care Importance

Recognizing the importance of stress management and mental health support, we must also emphasize that regular prenatal care is essential for monitoring and supporting the health of both mother and baby in AFFF-exposed pregnancies. Regular checkups play a pivotal role in tracking the baby's development, particularly in the context of AFFF exposure, which is known to pose risks to fetal health, including low birthweight.
Through prenatal care, healthcare providers can identify and manage potential risks or complications that may arise. These checkups are a cornerstone for providing personalized advice on mitigating medical, lifestyle, and environmental factors contributing to low birthweight in cases of AFFF exposure. Monitoring the baby's growth is essential, as it allows for the early detection of any signs of fetal growth restriction or other issues directly linked to AFFF exposure. This is critical because addressing these concerns promptly can alter the course of pregnancy and the baby's health outcomes.
Moreover, early detection and management of risk factors during prenatal visits can substantially reduce the likelihood of low birthweight in pregnancies impacted by AFFF. It's important for expectant mothers to maintain regular communication with their healthcare provider, ensuring that any concerns related to AFFF exposure and its potential impact on pregnancy are promptly and effectively addressed.
Genetic Vulnerabilities
In addition to environmental factors, genetic vulnerabilities greatly influence an individual's sensitivity to the adverse effects of AFFF contaminants. It's become increasingly clear that not everyone is affected by these contaminants in the same way. Research indicates that specific gene variations can profoundly alter how an individual's body processes and responds to the chemicals found in AFFF. This means that genetic factors are at the heart of determining individual susceptibility to the health impacts of exposure.
Variations in genes that are responsible for detoxification pathways are particularly vital. These genetic differences can impact how effectively the body can eliminate AFFF compounds, potentially leading to a greater accumulation of toxins in individuals with certain gene variations. This accumulation can worsen the health impacts of AFFF exposure, making it important to understand these genetic vulnerabilities.
Understanding these susceptibilities is not just an academic exercise; it has practical implications for interventions and treatments. By recognizing that some individuals are genetically more susceptible to the adverse effects of AFFF contaminants, we can tailor interventions to better protect these at-risk populations. This could involve more rigorous monitoring for health impacts, or perhaps even the development of targeted treatments that take into account an individual's genetic makeup.
Thus, our approach to managing the fallout from AFFF exposure must consider not only the environmental and prenatal factors but also the genetic vulnerabilities that affect individual susceptibility. By doing so, we can develop more effective interventions and ultimately mitigate the health impacts associated with AFFF contaminants.
Community Health Disparities

Community health disparities, particularly in low birthweight, underscore the urgent need for targeted interventions to support marginalized populations. We've observed that Black babies face higher rates of low birthweight compared to other ethnic groups. This fact alone highlights the deep-seated impact of systemic racism on pregnancy outcomes. It's clear that to address these disparities, we need strategies that specifically cater to the needs of these communities.
Factors such as socioeconomic status, limited access to healthcare, and environmental exposures play significant roles in influencing low birthweight rates across different demographics. It's evident that tackling these issues requires a multifaceted approach, focusing not only on the medical aspects but also on the social determinants of health. By promoting equity in healthcare access and addressing the root causes of these disparities, we can start to make a difference.
Effective strategies must consider the complex interplay between systemic racism, socioeconomic challenges, and environmental risks. It's about more than just providing medical care; it's about creating an environment where all expectant mothers have the resources and support they need for a healthy pregnancy. This involves a concerted effort from all sectors of society to make certain that interventions are not just targeted but also tailored to meet the unique needs of each community.
In short, addressing community health disparities in low birthweight is about recognizing the broader social and environmental factors at play. By focusing on these areas, we can work towards improving pregnancy outcomes for all, especially those in marginalized populations. It's not just a healthcare issue; it's a matter of social justice and equity.
Legal and Regulatory Context
Addressing health disparities in low birthweight also pushes us to confront the legal and regulatory challenges surrounding AFFF exposure. As we explore this aspect, it's essential to highlight the formation of multi-district litigation against AFFF manufacturers. This indicates a significant move towards legal action, underscoring the gravity of health risks tied to AFFF exposure. Plaintiffs across the board are stepping forward, filing lawsuits to hold manufacturers accountable for the continued production of AFFF despite the known risks.
The legal landscape is now marked with opportunities for those affected by AFFF exposure to seek compensation. This shift is not just about retribution; it's a clear message to manufacturers about the consequences of neglecting public health. The Dolman Law Group's specialization in firefighting foam lawsuits exemplifies the specialized legal support available to navigate these complex waters.
Our collective understanding of the situation demands a recognition of the legal remedies at hand. It's not just about acknowledging the health risks associated with low birth weight and AFFF exposure; it's about understanding that there's a pathway for those impacted to seek justice and compensation. This legal framework, while intricate, offers a beacon of hope for many, ensuring that the voices of the affected are heard and that manufacturers are held to account for their actions.
As we continue to unravel the implications of AFFF exposure, the legal and regulatory context provides a vital framework for addressing these challenges. It's a demonstration of the power of legal action in catalyzing change and offering hope to those affected by such profound health risks.
Future Research Directions
We must explore how AFFF exposure specifically leads to low birthweight in infants, setting the stage for important future research. Delving into the mechanisms at play will not only clarify the health effects of AFFF exposure but also pave the way for developing effective interventions. It's essential that we comprehend not just the immediate implications but also the long-term outcomes for infants subjected to such exposure in utero. This knowledge will help us craft strategies aimed at mitigating these risks and safeguarding future generations.
Investigating the role of genetic factors in conjunction with AFFF exposure in causing low birth weight is another avenue that promises valuable insights. By identifying genetic predispositions that may exacerbate the impact of AFFF, we can target our interventions more effectively, ensuring that those at greatest risk receive the most focused support.
Furthermore, fully understanding the dose-response relationship between AFFF exposure levels and low birthweight outcomes is essential. This information will be the cornerstone of developing targeted interventions that can prevent or at least reduce the risk of low birthweight in infants exposed to AFFF. It's about crafting a response that is as precise and effective as possible, minimizing the potential harm to our most vulnerable.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.