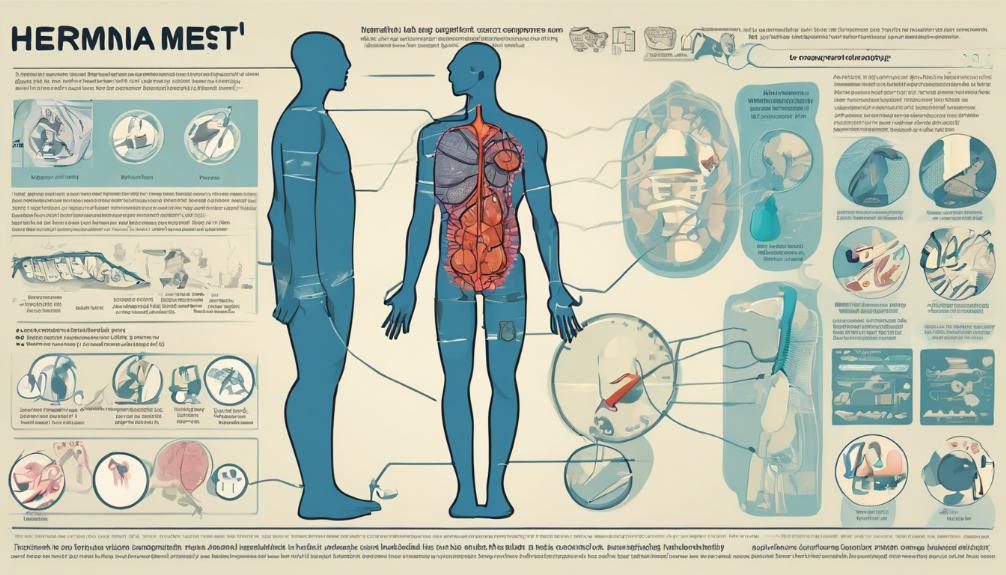
Surgical Mesh Used for Hernia Repair
The utilization of surgical mesh in hernia repair represents a cornerstone in modern surgical practices, offering a reinforcement mechanism that has significantly evolved over the years. As we navigate through the intricacies of hernia repair, the selection, application, and potential complications associated with various mesh materials become pivotal discussions within the medical community. These materials, ranging from synthetic to biologic, play a crucial role in the long-term outcomes of hernia surgeries. Examining the balance between the benefits of mesh reinforcement against the backdrop of potential post-surgical complications opens up a nuanced debate on its optimal use. This exploration invites a deeper examination into how current research and clinical evidence guide us towards making informed decisions in hernia repair strategies.

Understanding Hernias
A hernia is a medical condition characterized by the protrusion of an organ, intestine, or fatty tissue through a weak spot or hole in the surrounding muscle or connective tissue. Often manifesting at the abdominal wall, hernias can be visibly detected as an external bulge, particularly during activities that increase abdominal pressure such as coughing or lifting heavy objects. There are several types of hernias, including inguinal, femoral, incisional, ventral, and umbilical, each with distinct characteristics and locations within the body. The severity of hernias can vary widely, from small, asymptomatic cases to large, painful ones that require immediate medical attention. Understanding the nature and variety of hernias is crucial for effective diagnosis and management.
Causes and Risk Factors
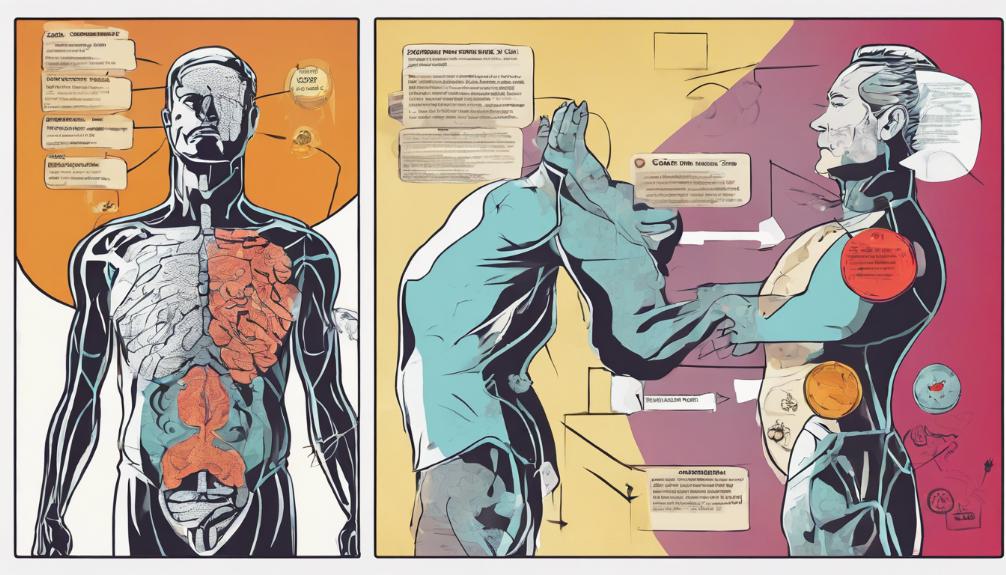
Understanding the development of hernias involves recognizing various causes and risk factors that contribute to the weakening of muscle or connective tissue. Hernias can arise from a combination of muscle weakness and increased pressure within the abdomen. This pressure can result from obesity, persistent coughing, heavy lifting, or even straining during bowel movements. Factors like poor nutrition, smoking, and previous surgical incisions can also predispose individuals to hernia development by compromising tissue integrity. Certain activities or conditions that elevate abdominal pressure significantly increase the risk. Moreover, age, genetics, and chronic medical conditions may play a role in the weakening of abdominal structures, making some individuals more susceptible to hernias than others. Understanding these factors is crucial for prevention and management strategies.
Treatment Options Explored
Exploring the range of treatment options is essential for effectively addressing hernia conditions, with strategies varying from conservative management to surgical intervention. For non-emergency cases, non-surgical options include monitoring the hernia for changes, lifestyle modifications to reduce strain on the affected area, and the use of abdominal binders for support. However, a significant percentage of hernias require surgical intervention to prevent complications such as obstruction or strangulation of the protruded organ. Surgical options range from open repair surgeries to minimally invasive techniques such as laparoscopic or robotic surgery. These procedures aim to repair the hernia by reinforcing the weakened area, with the choice of technique often depending on the hernia's size, location, and the patient's overall health.
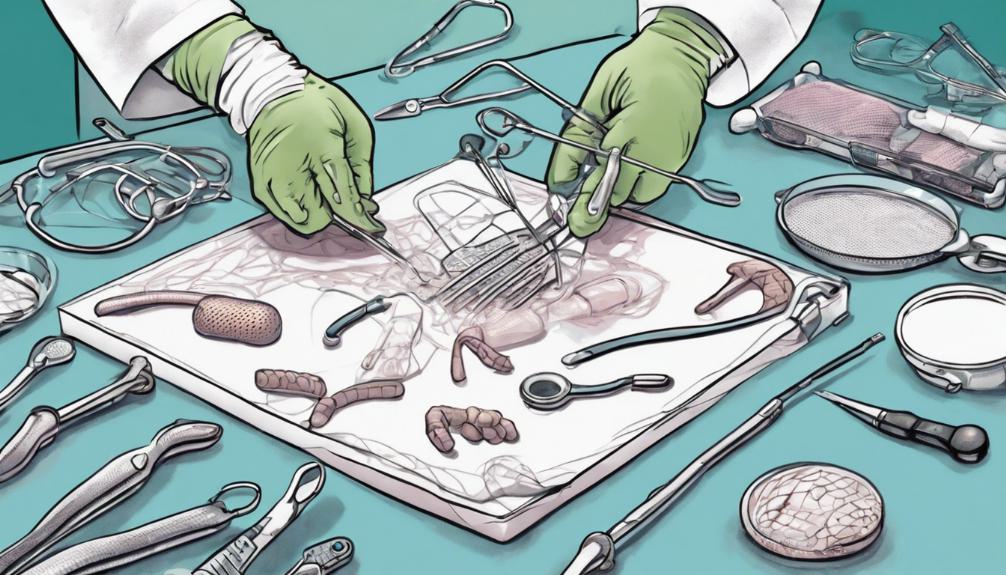
Role of Surgical Mesh
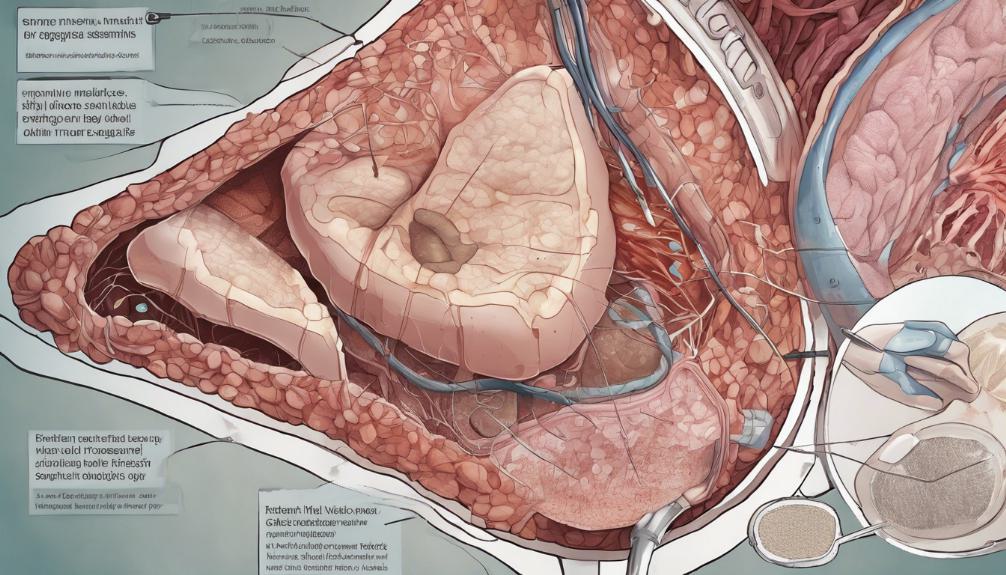
Surgical mesh, utilized in a majority of hernia repair surgeries, plays a pivotal role in providing support to weakened or damaged tissue. This medical device is indispensable in reinforcing areas where the hernia occurred, thereby significantly reducing the risk of recurrence. Its application spans various types of hernias, including inguinal, femoral, and incisional, among others. By acting as a scaffold, surgical mesh facilitates new tissue growth, ensuring the repair is more durable and resilient over time. Its integration into the repair process has been a breakthrough in surgical techniques, offering patients improved outcomes, shorter recovery times, and a marked decrease in the likelihood of hernia re-emergence. The strategic placement of surgical mesh is a critical component of successful hernia repair, underscoring its indispensable role in modern surgical practice.
Mesh Types and Durability
In hernia repair procedures, the choice of surgical mesh—ranging from synthetic to animal-derived, and from absorbable to non-absorbable—plays a crucial role in determining the durability and effectiveness of the surgery. Synthetic meshes, often made from materials like polypropylene or polyester, are favored for their long-term durability and resistance to infection. They are primarily used in non-absorbable mesh options, providing permanent support to the repaired area and significantly reducing the risk of recurrence. On the other hand, absorbable meshes, which gradually degrade and are absorbed by the body, offer temporary reinforcement, allowing time for the natural tissue to strengthen. Animal-derived meshes, typically made from processed and sterilized tissues of pigs or cows, offer an alternative for patients sensitive to synthetic materials, combining both durability and biocompatibility.
Frequently Asked Questions
How Do Patients Typically Recover After Hernia Repair Surgery That Involves the Use of Surgical Mesh?
Patients typically undergo a period of recovery following hernia repair surgery, which involves rest and gradual return to normal activities. The process may include pain management, wound care, and avoiding strenuous activities to facilitate healing. Recovery times can vary depending on the individual and the specific procedure performed. It is crucial for patients to follow their surgeon's post-operative instructions closely to ensure optimal healing and minimize the risk of complications or recurrence.
Can Surgical Mesh Cause Allergies or Reactions, and How Are Such Issues Managed?
Surgical mesh, utilized in various medical procedures, can potentially cause allergies or reactions in some patients. These adverse responses are typically managed through preoperative evaluations to identify any known sensitivities, selecting mesh materials that minimize risk, and closely monitoring postoperative signs of allergic reactions. In cases where reactions occur, treatment may include medications, such as antihistamines or corticosteroids, and in severe instances, removal of the mesh may be considered to alleviate symptoms.
What Are the Long-Term Outcomes and Potential Complications Years After a Hernia Repair With Mesh?
The long-term outcomes following hernia repair procedures generally aim for the permanent resolution of the hernia with minimal risk of recurrence. However, potential complications years after the operation can include chronic pain, infection, mesh migration, and hernia recurrence. The incidence of these complications varies based on factors such as the surgical technique used, the type of mesh, and the patient's overall health. Continuous follow-up is essential to monitor and address any long-term issues.
How Does the Choice Between Synthetic and Animal-Derived Mesh Affect the Surgery and Recovery Process?
The selection between synthetic and animal-derived mesh significantly influences both the surgical procedure and the recovery process. Synthetic meshes, often made from materials like polypropylene, provide durable, long-term reinforcement. In contrast, animal-derived meshes, typically sourced from bovine or porcine tissues, offer a natural alternative that may be better tolerated by some patients but might not last as long. Each type has distinct implications for tissue integration, potential for infection, and overall recovery trajectory.
Are There Any Advancements or Innovations in Surgical Mesh Technology That Might Benefit Future Hernia Repairs?
Recent advancements in surgical mesh technology show promise for enhancing future hernia repair procedures. Innovations focus on improving biocompatibility, reducing infection risks, and promoting tissue integration. New materials and manufacturing techniques aim to create meshes that better mimic the body's natural movements and reduce foreign body sensation. These developments could lead to more effective and comfortable treatments for patients, potentially decreasing the likelihood of recurrence and improving overall surgical outcomes.

This post has been generated by AI and was not reviewed by editors. This is Not legal advice. Please consult with an attorney.




